To investigate the association between the duration of the first prone positioning maneuver (PPM) and 90-day mortality in patients with C-ARDS.
DesignRetrospective, observational, and analytical study.
SettingCOVID-19 ICU of a tertiary hospital.
PatientsAdults over 18 years old, with a confirmed diagnosis of SARS-CoV-2 disease requiring PPM.
InterventionsMultivariable analysis of 90-day survival.
Main variables of interestDuration of the first PPM, number of PPM sessions, 90-day mortality.
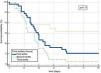
Results271 patients undergoing PPM were analyzed: first tertile (n = 111), second tertile (n = 95) and third tertile (n = 65). The results indicated that the median duration of PDP was 14 h (95% CI: 10−16 h) in the first tertile, 19 h (95% CI: 18−20 h) in the second tertile and 22 h (95% CI: 21−24 h) in the third tertile. Comparison of survival curves using the Logrank test did not reach statistical significance (p = 0.11). Cox Regression analysis showed an association between the number of pronation sessions (patients receiving between 2 and 5 sessions (HR = 2.19; 95% CI: 1.07–4.49); and those receiving more than 5 sessions (HR = 6.05; 95% CI: 2.78–13.16) and 90-day mortality.
Conclusionswhile the duration of PDP does not appear to significantly influence 90-day mortality, the number of pronation sessions is identified as a significant factor associated with an increased risk of mortality.
investigar la asociación entre la duración de la primera maniobra de posición en decúbito prono (PDP) y la mortalidad a 90 días en pacientes con C-ARDS.
Diseñoestudio retrospectivo, observacional y analítico.
ÁmbitoUCI-COVID de hospital terciario.
Pacientesmayores de 18 años, con diagnóstico confirmado de enfermedad por de SARS-CoV-2 que necesitaron de maniobra de PDP.
Intervencionesanálisis multivariable de supervivencia a 90 días.
Variables de interés principalesduración de la primera PDP, número de sesiones de PDP, mortalidad a 90 días.
Resultados271 pacientes sometidos a PDP fueron analizados: primer tercil (n = 111), segundo tercil (n = 95) y tercer tercil (n = 65). Los resultados indicaron que la mediana de la duración del PDP fue de 14 horas (IC95%: 10−16 horas) en el primer tercil, 19 horas (IC95%: 18−20 horas) en el segundo tercil y 22 horas (IC95%: 21−24 horas) en el tercer tercil. La comparación de las curvas de supervivencia a través de la prueba de Logrank, no alcanzó significancia estadística (p = 0,11). El análisis de Regresión de Cox evidenció asociación entre el número de sesiones de pronación (los pacientes que recibieron entre 2 y 5 sesiones (HR = 2,19; IC 95%: 1,07−4,49); y aquellos que recibieron más de 5 sesiones (HR = 6,05; IC 95%: 2,78−13,16) y la mortalidad a 90 días.
Conclusionesmientras que la duración del PDP no parece influir de forma significativa en la mortalidad a 90 días, el número de sesiones de pronación se identifica como un factor significativo asociado con un mayor riesgo de mortalidad.
Acute respiratory distress syndrome caused by SARS-CoV-2 (hereinafter referred to as C-ARDS [COVID-acute respiratory distress syndrome]) has given rise to an unprecedented worldwide health crisis, with high morbidity and mortality, particularly in patients with acute respiratory failure. In this context, prone position maneuvering (PPM) has proven to be a crucial therapeutic measure for improving oxygenation and lung mechanics in critically ill patients.1–5
However, despite its widespread use in clinical practice, the optimum duration of the first PPM session in patients with C-ARDS has not been clearly established to date. In addition to this lack of consensus, there is little evidence on the specific impact of the initial duration of PPM upon the long-term clinical outcomes.6–9
In this context, it has been suggested that the duration of the first PPM session may significantly influence middle-term mortality among patients with C-ARDS. It has been postulated that an optimum duration of the first session could result in improved oxygenation and an alleviation of pulmonary stress, favoring more effective pulmonary recovery and reducing the incidence of serious respiratory complications, with a consequent decrease in mortality.10–14
The present study was carried out to explore the association between the duration of the first PPM session and 90-day mortality among patients with C-ARDS. For this purpose, the patients were divided into time tertiles according to the duration of the first PPM session, and an analysis was made of the clinical outcomes, focusing particularly on 90-day mortality.
Material and methodsA retrospective, observational analytical study was carried out involving the adults admitted to the COVID-19 area with a diagnosis of SARS-CoV-2 infection confirmed by respiratory tract cell polymerase chain reaction (PCR) testing in the Department of Intensive Care Medicine of a tertiary hospital between March 2020 and March 2022. The data were collected from the COVID-19 patient registry in the Department of Intensive Care Medicine. The study was approved by the local Research Ethics Committee (reference code 2020.250), and informed consent to use of the data was obtained from the patients or their legal representatives in writing and/or verbally by telephone. Some data that were not initially collected were later obtained on a retrospective basis.
Inclusion criteria: patients over 18 years of age, with a diagnosis of SARS-CoV-2 disease confirmed in the first 24 h of hospital stay; need for admission to the Intensive Care Unit (ICU) due to respiratory failure, with mechanical ventilation (MV); need for PPM as part of the management of respiratory failure. Exclusion criteria: data registries containing errors in the study variables; use of PPM in awake patients. The recorded variables are described in more detail in the supplementary material.
The patients were divided into tertiles according to the duration (in hours) of the first PPM session. The indication of the latter, as well as cessation of the maneuver, was decided by the supervising physician based on the recommendations for the management of critically ill patients with COVID-19 in ICUs of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]), which propose a duration of PPM of at least 16 h.15 Early PPM was defined as those patients placed in the prone position within the first 24 h following admission.
The patients were followed up on for 90 days from the moment of admission to the ICU or until death (whichever occurred first).
We performed a first descriptive analysis of the sample, reporting categorical variables as absolute values and percentages, with calculation of the median and percentiles 25−75 (p25−75) in the case of continuous quantitative variables. The comparison of percentages between groups was carried out based on contingency tables and the chi-square test. The Kruskal-Wallis test was used in the case of continuous variables.
Subsequently, a multivariate survival analysis was performed, with adjustment of a Cox regression model (method: forward stepwise, entering variables in the model if p < 0.05 and excluding them if p > 0.2; status: 90-day mortality, selecting the independent variables with p < 0.2 in the bivariate analysis). Associations were expressed using the hazard ratio (HR) with the corresponding 95% confidence interval (95%CI). Harrell’s C-index was used to assess concordance in the Cox regression model. Statistical significance was considered for p < 0.05 in all the tests.
The analysis of 90-day survival was based on the Kaplan-Meier method for the variable time of death (log-rank test).
ResultsA total of 911 patients were admitted to the COVID-19 ICU during the study period. With a total of 894 analyzed patients (Table 1), we evaluated the distribution of cases in the course of the different waves of the pandemic, with the sixth wave making the greatest contribution to the number of patients (24.5%). A total of 300 patients (33%) were subjected to some PPM sessions during their ICU stay. After filtering the data, we analyzed a total of 271 patients subjected to PPM. Most of the patients (n = 111, 41%) were classified into the first tertile of the duration (in hours) of the first PPM session, 95 (35%) in the second tertile, and 65 (24%) in the third tertile (Fig. 1).
Main variables of the study cohort.
| Total patients n = 894 | |
|---|---|
| Time period of pandemic | |
| 1st wave, n (%) | 67 (7.5%) |
| 2nd wave, n (%) | 161 (18%) |
| 3rd wave, n (%) | 185 (27%) |
| 4th wave, n (%) | 130 (14.5%) |
| 5th wave, n (%) | 130 (14.5%) |
| 6th wave, n (%) | 221 (24.5%) |
| Age (years), median (p25−75) | 64 (53−72) |
| Male gender, n (%) | 624 (70%) |
| AHT, n (%) | 392 (44%) |
| Obesity, n (%) | 146 (16%) |
| Diabetes, n (%) | 174 (19%) |
| Dyslipidemia, n (%) | 197 (22%) |
| Smoker, n (%) | 266 (30%) |
| SOFA score, median (p25-p75) | 5 (4−6) |
| The main reason for admission ARF, n (%) | 775 (88%) |
| PaO2/FiO2 upon admission to ICU, mmHg, median (p25-p75) | 146 (114−187) |
| Need for IMV, n (%) | 571 (64%) |
| Prone position therapy, n (%) | 300 (33%) |
| Corticosteroid use, n (%) | 654 (73%) |
| Days on MV, median (p25–p75) | 9 (5−16) |
| ICU stay (days), median (p25–p75) | 9 (4−17) |
PaO2/FiO2: ratio of arterial oxygen partial pressure to the fraction of inspired oxygen; AHT: arterial hypertension; HFOT: high-flow oxygen therapy, MV: mechanical ventilation; ARF: acute respiratory failure. SOFA: Sequential Organ Failure Assessment.
The median duration of PPM was 14 h (95%CI: 10−16) in the first tertile, 19 h (95%CI: 18−20) in the second tertile, and 22 h (95%CI: 21−24) in the third tertile.
The comparative analysis of the clinical-epidemiological characteristics, grouped by time tertiles (in hours) of the first PPM session, evidenced uniformity in the presentation of cases in the course of the different waves, with certain variations in biomarkers and vaccination status (Table 2). C-reactive protein (CRP) showed significant variations between groups (p = 0.02), and chronic renal failure (CRF) was more pronounced in the patients belonging to the first tertile (p = 0.04) (Table 2).
Comparison of the clinical-epidemiological characteristics of the patients according to time tertiles (hours) of the first PPM session.
| First tertile 14 h (95%CI: 10−16)n = 111 | Second tertile19 h (95%CI: 18−20) n = 95 | Third tertile22 h (95%CI: 21−24) n = 65 | p | |
|---|---|---|---|---|
| Time period of pandemic | ||||
| 1st wave, n (%) | 17 (15%) | 8 (8%) | 12 (18%) | 0.36 |
| 2nd wave, n (%) | 21 (19%) | 29 (30%) | 14 (21%) | |
| 3rd wave, n (%) | 29 (26%) | 30 (31%) | 15 (23%) | |
| 4th wave, n (%) | 17 (15%) | 7 (7%) | 10 (15%) | |
| 5th wave, n (%) | 10 (9%) | 9 (9%) | 6 (9%) | |
| 6th wave, n (%) | 17 (15%) | 12 (13%) | 8 (12%) | |
| Comorbidities | ||||
| Age (years), median (p25−75) | 63 (55−70) | 65 (56−72) | 65 (53−70 | 0.65 |
| Male gender, n (%) | 79 (71%) | 67 (70%) | 47 (72%) | 0.97 |
| Vaccination status: | ||||
| Complete, n (%) | 4 (4%) | 1 (1%) | 1 (1%) | 0.63 |
| Incomplete, n (%) | 11 (10%) | 9 (9%) | 4 (6%) | |
| Not vaccinated, n (%) | 96 (86%) | 85 (89%) | 60 (92%) | |
| AHT, n (%) | 58 (52%) | 42 (44%) | 26 (40%) | 0.25 |
| Obesity, n (%) | 24 (22%) | 18 (19%) | 10 (15%) | 0.60 |
| Diabetes, n (%) | 19 (17%) | 19 (20%) | 14 (21%) | 0.75 |
| Dyslipidemia, n (%) | 39 (35%) | 21 (22%) | 19 (29%) | 0.12 |
| Smoker, n (%) | 45 (40%) | 30 (31%) | 22 (34%) | 0.38 |
| OH abuse, n (%) | 12 (11%) | 6 (6%) | 4 (6%) | 0.40 |
| CRF, n (%) | 10 (9%) | 5 (5%) | 0 (0%) | 0.04 |
| SOFA, median(p25–p75) | 5 (4−6) | 5 (4−6) | 5 (4−6) | 0.95 |
| Studied biomarkers | ||||
| CK (median p27−75) | 125 (55−261) | 110 (52−318) | 221 (71−371) | 0.23 |
| D-dimer(median p27−75) | 926 (583−2149) | 980 (646−1773) | 991 (555−3621) | 0.94 |
| Ferritin(median p27−75) | 803 (461−1370) | 1004 (485−1428) | 994 (617.25−1526) | 0.55 |
| IL-6 (median p27−75) | 103 (35−135) | 69 (17−135) | 65 (31−108) | 0.18 |
| CRP, mean (SD) | 16 (7−22) | 10 (5−18) | 13 (8−24) | 0.02 |
| Troponin (median p25−75) | 18 (6−48) | 13 (7−41) | 19 (10−61) | 0.77 |
| LDH (median p27−75) | 403 (327−505) | 402 (322−475) | 396 (313−513) | 0.67 |
AHT: arterial hypertension; CRF: chronic renal failure; OH: alcohol. SOFA: Sequential Organ Failure Assessment.
There were differences in clinical presentation and treatment strategies according to the tertile involved (Table 3). The ratio of arterial oxygen partial pressure to the fraction of inspired oxygen (PaO2/FiO2) showed significant variations, with lower values in the first tertile (p < 0.05), and there were different patterns in the use of nasal high-flow oxygen therapy (HFOT) in the UCI, with a significant decrease in its use among the patients in which the first PPM session was longest (third tertile) (p = 0.05). In turn, the use of extracorporeal membrane oxygenation (ECMO) showed variability, though without reaching statistical significance (p = 0.09). The median number of PPM sessions was 2, with an interquartile range (IQR) of 1−4 sessions in all the groups. In terms of frequency, approximately one-third of the patients underwent a single PPM session. The differences between groups were not statistically significant (p = 0.11).
Comparative analysis between time tertiles (hours) of the first PPM session referred to the main variables associated with acute respiratory failure and therapeutic interventions in the ICU.
| First tertile 14 h (95%CI: 10−16)n = 111 | Second tertile19 h (95%CI: 18−20) n = 95 | Third tertile22 h (95%CI: 21−24) n = 65 | p | |
|---|---|---|---|---|
| ARF as the main reason for admission to ICU, n (%) | 110 (94%) | 94 (98%) | 64 (98%) | 0.92 |
| Variables and therapeutic interventions related to respiratory failure | ||||
| PaO2/FiO2 upon admission to ICU, mmHg, median (p25−75) | 120 (91−144) | 142 (106−169) | 120 (86−147) | <0.05 |
| Previous use of HFOT in ICU, n (%) | 50 (45%) | 49 (52%) | 21 (32%) | 0.05 |
| Hours of HFOT, median (p25−75) | 45 (17−72) | 46 (14−72) | 15 (11−24) | 0.02 |
| PaO2/FiO2 prior to MV, mmHg, median (p25−75) | 100 (87−120) | 105 (87−135) | 100 (80−130) | 0.43 |
| Days ICU-PPM, median (p25−75) | 1 (1−2) | 1 (1−3) | 1 (1−2) | 0.25 |
| PaO2/FiO2 prior to PPM, median (p25−75) | 124 (97−156) | 120 (100−150) | 127 (103−150 | 0.73 |
| Duration (hours) PPM, median (p25−75) | 14 (10−16) | 19 (18−20) | 22 (21−24) | <0.05 |
| Early prone position, n (%) | 78 (70%) | 59 (62%) | 46 (70%) | 0.37 |
| Number of PPM sessions, median (p25-75) | 2 (1-4) | 2 (1-4) | 2 (1-4) | 0.95 |
| Frequency PPM session, n (%) | ||||
| Single session | 38 (34%) | 33 (35%) | 18 (28%) | |
| 2–5 sessions | 56 (50%) | 52 (55%) | 38 (58 %) | |
| >5 sessions | 17 (15%) | 10 (10%) | 9 (14%) | |
| Initial ventilatory parameters | ||||
| Tidal volume (ml), median (p25−75) | 470 (450−485) | 475 (450−490) | 480 (450−500) | 0.55 |
| BR (rpm), median (p25−75) | 18 (16−20) | 18 (16−18) | 18 (16−20) | 0.65 |
| PEEP, cmH2O, median (p25−75) | 10 (10−12) | 10 (8−12) | 12 (10−13) | 0.24 |
| Pplateau, cmH2O, median (p25−75) | 22 (20−26) | 23 (21−25) | 22 (21−25) | 0.69 |
| DP, cmH2O, median (p25−75) | 10 (9−14) | 11 (9−14) | 11 (8−14) | 0.74 |
| Mechanical power, J/min, median (p25−75) | 17 (15−21) | 18 (14−20) | 18 (16−20) | 0.44 |
| Therapies used for SARS-CoV-2 | ||||
| Remdesivir, n (%) | 9 (8%) | 12 (13%) | 6 (9%) | 0.54 |
| Corticosteroids, n (%) | 92 (83%) | 84 (88%) | 57 (88%) | 0.47 |
| Tocilizumab, n (%) | 32 (29%) | 27 (28%) | 18 (28%) | 0.99 |
| Plasma, n (%) | 32 (29%) | 28 (29%) | 16 (25%) | 0.78 |
| Therapies used during ICU stay | ||||
| Vasoactive drugs, n (%) | 71 (64%) | 56 (59%) | 36 (55%) | 0.51 |
| CRRT, n (%) | 7 (6%) | 5 (5%) | 5 (8%) | 0.97 |
| ECMO, n (%) | 5 (4%) | 1 (1%) | 0 (0%) | 0.09 |
| iNO, n (%) | 10 (9%) | 12 (13%) | 8 (12%) | 0.67 |
ARDS: acute respiratory distress syndrome; PaO2/FiO2: ratio of arterial oxygen partial pressure to the fraction of inspired oxygen, HFOT: high-flow oxygen therapy, MV: mechanical ventilation; CRRT: continuous renal replacement therapy; ECMO: extracorporeal membrane oxygenation; iNO: inhaled nitric oxide; BR: breathing rate; DP: driving pressure.
In the analysis of the main evolutive variables between the groups (Table 4), no significant differences were found in terms of either the duration of MV or the duration of ICU stay (p = 0.74 and p = 0.88, respectively). The diagnosis of ventilator-associated tracheobronchitis/pneumonia (VAT/VAP) tended to be more prevalent in the second tertile (64%) (p = 0.08). Other study outcomes, such as the diagnosis of massive pulmonary thromboembolism (PTE), and the need for tracheostomy, showed no substantial differences.
Main evolutive variables analyzed between the different groups according to time tertile (hours) of the first PPM session.
| First tertile 14 h (95%CI: 10−16)n = 111 | Second tertile19 h (95%CI: 18−20) n = 95 | Third tertile22 h (95%CI: 21−24) n = 65 | p | |
|---|---|---|---|---|
| Days on MV, median (p25–p75) | 14 (7−24) | 13 (8−25) | 12 (8−19) | 0.74 |
| ICU stay (days),median (p25–p75) | 17 (10−27) | 17 (10−30) | 15 (10−27) | 0.88 |
| Diagnosis of VAT/VAP, n (%) | 62 (56%) | 61 (64%) | 30 (46%) | 0.08 |
| Diagnosis of massive PTE, n (%) | 7 (6%) | 4 (4%) | 3 (5%) | 0.77 |
| Need for tracheostomy, n (%) | 22 (20%) | 20 (21%) | 11 (17%) | 0.81 |
| 90-day mortality | 27 (24%) | 27 (28%) | 9 (14%) | 0.10 |
MV: mechanical ventilation; ICU: Intensive Care Unit; VAT/VAP: ventilator-associated tracheobronchitis/pneumonia; PTE: pulmonary thromboembolism.
The survival analysis showed a mean survival of 74 days with a standard error (SE) of 2.687 and a 95%CI of 69–79 days in the first tertile. In the second tertile, the mean survival was slightly lower (71 days, SE 3.191; 95%CI: 64–77 days). In contrast, the third tertile showed the highest mean survival (80 days, SE 3.085; 95%CI: 74–86 days). Based on the Kaplan-Meier method and comparing the survival curves using the log-rank test, no statistical significance was observed (p = 0.11), though the patients with the longest duration of the first PPM session tended to present greater survival (Fig. 2).
Lastly, in the Cox regression analysis referred to survival time over the 90 days of follow-up, the model included variables such as patient age, where a one-year increase in age was seen to be associated with a 7.07% increase in 90-day mortality risk (HR = 1.07; 95%CI: 1.03–1.10). In turn, those patients who required ECMO had a 4.42-fold higher mortality risk than those who did not need ECMO (HR = 4.42; 95%CI: 1.52–12.82). The number of PPM sessions was also significantly correlated to 90-day survival: those patients receiving between 2−5 sessions had a 2.19-fold higher mortality risk than those who underwent a single PPM session (HR = 2.19; 95%CI: 1.07–4.49), and those who received > 5 sessions had an even mortality higher risk (6.05-fold) versus the reference group (HR = 6.05; 95%CI: 2.78–13.16). In turn, PaO2/FiO2 upon admission to the ICU was also significantly correlated to survival: for each unit increase in PaO2/FiO2, 90-day survival was seen to increase 0.68% (HR = 1.00; 95%CI: 1.00–1.01). Harrell’s C-index was 0.745 (95%CI: 0.68−0.80). The following variables were not included in the model: gender, CRP level, IL-6, VAT/VAP, CRF, the use of HFOT, the duration of HFOT and the different time tertiles of the first PPM session.
DiscussionThe present study did not show patients with the longest first PPM sessions to have significantly greater 90-day survival, though the results obtained suggest the need to further explore the impact of PPM time upon the clinical course of patients with C-ARDS. On the other hand, the number of PPM sessions was seen to be significantly associated with 90-day mortality, with the lowest mortality risk corresponding to those individuals subjected to a single PPM session.
Although we recorded no differences in specific complications during ICU stay capable of accounting for the observed differences in the survival curves from the second week of follow-up, it is important to consider that other factors not evaluated in the study could have influenced patient mortality, such as additional comorbidities, post-ICU treatment, the quality of the care provided, or unknown middle-term complications. For example, modification of the work structure, along with other factors, could have exerted an arbitrary influence upon the moment in which intubation was decided and mechanical ventilation with protective strategies was started, and on the adoption of maneuvers such as prone positioning. We found that in those cases where the duration of the first PPM session was longer, the use of HFOT before MV was also greater – a situation that can cause delays in intubation, which as we know may result in a poorer prognosis.16,17
The clinical rationale for extending the duration of the PPM sessions is based on the main benefit of this position, which results in more uniform stress and tension applied by mechanical ventilation in the lungs. The prone position favors a more uniform distribution of the ventilation volume. Studies have shown that PPM can improve the homogenization of pleural pressure and reopening of the posterior alveolar units. From the organizational perspective, extending the PPM sessions to over 24 h can significantly reduce the workload, and the risk of complications associated with frequent rotation and viral exposure. In addition, it could increase adherence to the prone position by concentrating the returns to the supine position during the day, thereby improving the safety of the procedure. However, extending the duration of PPM is not without risks, such as an increased risk of pressure sores, more catheter-related incidents, the interruption of enteral nutrition, plexus disorders or paralysis of the brachial plexus, among other conditions.18
In our study, the decision to divide the patients into tertiles was based on greater sensitivity to data variation (of advantage in capturing differences between values with greater detail), simplification of the interpretation and reporting of results, usefulness in analyzing or highlighting differences in the distributions, and the facility of comparing groups between tertiles: an intermediate duration group with two comparator groups (from longer to lesser duration).19
It is important to underscore that apart from the application of protective mechanical ventilation, the failure of the first studies to demonstrate survival benefit with PPM in ARDS has been attributed to both an insufficient duration of PPM and to a late start of PPM.20–22 The recommendations of the SEMICYUC for the management of critically ill patients with COVID-19 in the ICU established a duration of PPM of at least 16 h.15 These recommendations were mainly based on the work of Guerin et al.,1 who documented a marked decrease in mortality from 41% to 23.6% (p = 0.001) on applying PPM sessions (4 days) lasting 17 h in patients with a mean PaO2/FiO2 of 100 ± 30 mmHg and protective ventilation (tidal volume 6 ml/kg).
However, the number of patients requiring PPM increased during the pandemic, and as a consequence of care overload or of increased severity of the disease, some patients remained on PPM for longer periods18 – what some authors refer to as extended PPM. However, extended PPM had already been described before the pandemic in small pseudorandomized studies23 and retrospective single-center studies in which sample heterogeneity, the few patients involved, and the differences in positive end-expiratory pressure (PEEP) as criteria for ending the sessions and follow-up, did not allow conclusions to be drawn in relation to patient survival.24–26 Nevertheless, many of these studies reported marked improvements in oxygenation among patients with extended PPM versus the more conventional maneuvers.
During the pandemic, several centers published their experience with extended PPM in patients with C-ARDS subjected to mechanical ventilation. The most relevant studies highlight the importance of the organizational strategies employed, such as the “two nights” protocol, with a median PPM duration of 39 h (interquartile range 34–42). This protocol allowed an increase in PaO2/FiO2 during the first PPM session that was associated with a decrease in mortality in the ICU. On the other hand, clinical strategies were also established: once PPM was started, it was maintained until clinical improvement was achieved. The alternation between PPM and the supine position was suppressed entirely. This strategy was first described on a large scale in C-ARDS by Douglas et al.27 The PPM sessions were maintained until the patients met the following criteria: PaO2/FiO2 > 150 with FiO2 > 60% and PEEP < 10 cmH2O. This protocol resulted in sessions with a median duration of 2.95 days among the survivors and 3.3 days among the non-survivors. In one-quarter of the latter cases, the sessions lasted at least 6.6 days.
Lastly, a single study explored the causal relationship between the clinically guided duration of PPM and mortality.28 This was a retrospective multicenter study involving a total of 263 patients. The median duration of PPM in the extended PPM group was 40 h, and the maximum duration of a single session was over 10 days. The median duration of PPM in the standard duration PPM group was 17 h. The patients in the extended PPM group had a lower three-month mortality rate than the patients in the standard duration group (HR: 0.47; 95%CI: 0.34–0.67; p < 0.001).
In a study exclusively focused on the first PPM cycle, González et al.29 analyzed the characteristics, changes in oxygenation and lung mechanics of patients with C-ARDS subjected to PPM, with evaluation of the response to the first maneuver. The mortality rate was seen to be significantly lower in those individuals presenting an increase in oxygenation after PPM. Patient age, the percentage increase in PaO2/FiO2 after 24 h of PPM and the number of cycles were identified as independent factors related to mortality.
In our setting, Miguel Balsa et al.30 described the characteristics of patients with C-ARDS subjected to invasive mechanical ventilation (IMV), and analyzed the effect of prolonged PPM (over 24 h) versus PPM for less than 24 h. Extended PPM was seen to be associated with less tolerance of ventilation in the supine position, longer hospital stay, more days of IMV, a longer duration of neuromuscular block treatment, and a greater number of orotracheal tube obstruction episodes.
Based on the results of our analysis and the literature review, it might be postulated that extending PPM beyond 16 h – which is currently the predominant recommendation – could prove feasible in terms of survival. However, the best approach for extending this duration remains to be defined: a fixed duration established by the care organization, or the application of clinical criteria to decide the end of PPM? Further prospective and interventional investigations are clearly needed to evaluate these aspects more in-depth.
In addition to the limitations inherent to its retrospective nature, our study has the limitation of indicating PPM based on the criterion of the supervising physician, without a fixed and standardized protocol. Nevertheless, no significant differences were observed in the variables related to the time of indication, which suggests that variability in medical decision-making had no statistically significant impact on the results obtained. The lack of data referred to oxygenation and lung mechanics justifying the suspension of the maneuvers also partly limited the study. On the other hand, some of the variables not entered into the model could strongly correlate to other predictive variables already included. Another limitation that needs to be mentioned is the percentage loss of patients during follow-up. We found that approximately 10% of the patients subjected to prone positioning (29 out of 300) were lost during the study, and it is not possible to establish whether these losses were random or were influenced by specific factors such as the severity of the disease or the particular moment during the pandemic. The possibility of bias in the selection of the lost patients could have implications for the interpretation of our results and the generalization of the findings obtained. In addition, mention must be made of the effect of imprecision of the estimations, given the sample size involved. We acknowledge that because of the nature of the study and the size of the sample, there may be limitations in the precision of our results. Lastly, it is important to note that the justification for early suspension of the first PPM session was not documented: such justification was not possible, since some patients included in the first tertile received an insufficient duration of PPM according to the PROSEVA study.1
Conflict of interestAll the authors declare that they have no conflicts of interest.
Authors’ contributionsAll the signing authors meet the requirements of authorship and all of them declare that they have no conflicts of interest. The study complies with the principles of Good Clinical Practice. All author rights are transferred to the journal MEDICINA INTENSIVA in the event that the article is accepted for publication:
Alejandro González-Castro: Conception, development and writing of the manuscript.
Elena Cuenca-Fito: Data compilation.
Yhivian Peñasco: Development, correction.
Carmen Huertas: Filtering of database.
Camilo Gonzalez: Writing and correction.
Juan Carlos Rodríguez-Borregán: Writing and correction.
The present study has received no financial support.