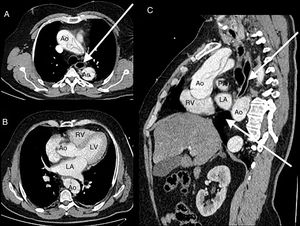
Fifty-seven-year-old male with a past medical history of high blood pressure and hiatal hernia admitted to the ER with clinical signs of syncope and chest pain. He is diagnosed with a Stanford type A aortic dissection and immediately referred to urgent surgery. After the intervention, the patient is admitted to the Intensive Care Unit. In order to guarantee enteral nutrition a nasogastric tube is inserted with difficulties when trying to move the tube forward. Its positioning is verified through the use of contrast and its malposition is eventually confirmed (Fig. 1). The thoracic coronary CT angiography shows a dissection-induced aortic hematoma causing an extrinsic esophageal compression with progressive tapering and dilatation prior to the obstruction (Fig. 2). Eventually, the patient requires endoscopic implantation to resolve the esophageal stenosis.
Thoracoabdominal CT scan. A. Pre-stenotic axial image showing the esophageal dilatation and aortic dissection. B. Axial image of the compression region (white asterisk). C. Coronal imaging showing progressive esophageal tapering.Ao, aorta with image of aortic flap; LA, left atrium; LV, left ventricle; PA, pulmonary artery; RV, right ventricle. White arrow: pre- and post-stenotic esophageal dilatation. White asterisk: esophageal obstruction region.
We wish to thank the Radiology unit of the Hospital Universitario 12 de Octubre for their collaboration.
Please cite this article as: Valiente Fernández M, Czapka Mital JD, Pérez Vela JL. Estenosis esofágica secundaria a disección aórtica. Med Intensiva. 2019. https://doi.org/10.1016/j.medin.2019.02.003