(1) To assess the prevalence of pain during nursing care procedures, and (2) to evaluate the usefulness of certain vital signs and the bispectral index (BIS) in detecting pain.
MethodsA prospective, observational analytical study was made of procedures (endotracheal aspiration and mobilization with turning) in critically ill sedated patients on mechanical ventilation. The Behavioral Pain Scale was used to assess pain, with scores of ≥3 indicating pain. Various physiological signs and BIS values were recorded, with changes of >10% being considered clinically relevant.
ResultsA total of 146 procedures in 70 patients were analyzed. Pain prevalence during the procedures was 94%. Vital signs and BIS values increased significantly during the procedures compared to resting conditions, but only the changes in BIS were considered clinically relevant. In the subgroup of patients receiving preemptive analgesia prior to the procedure, pain decreased significantly compared to the group of patients who received no such analgesia (−2 [IQR: {−5}–0] vs. 3 [IQR: 1–4]; P<.001, respectively).
ConclusionsThe procedures evaluated in this study are painful. Changes in vital signs are not good indicators of pain. Changes in BIS may provide useful information about pain, but more research is needed. The administration of preemptive analgesia decreases pain during the procedures.
1) Evaluar la prevalencia de dolor durante 2 procedimientos de enfermería, y 2) analizar la utilidad de ciertos signos vitales y del índice biespectral (BIS) para detectar dolor.
MétodosEstudio prospectivo, observacional y analítico de medidas repetidas en pacientes con ventilación mecánica y sedación. Los procedimientos evaluados fueron la aspiración endotraqueal y la movilización con giro. El dolor se evaluó mediante la Behavioral Pain Scale. Valores≥3 se consideraron dolorosos. Se registraron distintos signos fisiológicos y los valores del BIS. Una variación porcentual>10% se consideró clínicamente relevante.
ResultadosSe analizaron 146 procedimientos en 70 pacientes. La prevalencia de dolor durante los procedimientos fue del 94%. Los signos vitales y los valores del BIS aumentaron significativamente durante los procedimientos respecto el reposo, pero solo la variación del BIS alcanzó relevancia clínica. En un subgrupo de pacientes que recibieron analgesia preventiva antes de los procedimientos, el dolor disminuyó significativamente respecto a los pacientes que no recibieron analgesia preventiva (−2 [RIQ: {−5}-0] vs. 3 [RIQ: 1–4]; p<0,001, respectivamente).
ConclusionesLos procedimientos evaluados son dolorosos. La variación de los signos vitales no es un buen indicador de dolor. La variación del BIS podría ser útil, pero precisa nuevas investigaciones. La administración de analgesia preventiva disminuye la prevalencia de dolor durante los procedimientos.
Between 50 and 70% of all patients admitted to the Department of Intensive Care Medicine (DICM) experience pain.1,2 Furthermore, pain has relevant consequences in the critical patient. Apart from ethical considerations, pain is the most unpleasant memory patients describe upon discharge from the DICM.3 On the other hand, the presence of pain during admission to the DICM is associated to an increased incidence of chronic pain4, posttraumatic stress syndrome5 and, in general, poorer quality of life6.
Pain may be due to a number of causes, such as the background disease process or monitoring techniques and/or nursing care procedures, which are frequent and unavoidable. Puntillo et al.7 evaluated the perception of pain in over 6000 conscious critical patients subjected to 6 procedures: mobilization with turning, the placement of central venous catheters, the removal of chest drains, wound cures, endotracheal aspiration, and the removal of femoral arterial catheters. The authors concluded that all these procedures were painful, and that mobilization was the most painful procedure of all.
The main reason for not diagnosing–and therefore not treating–pain is failure to detect the problem.1,2 Self-evaluation is the best way to assess pain in the conscious patient.8 However, many patients admitted to the DICM are unable to communicate for different reasons: altered level of consciousness, mechanical ventilation (MV) and/or the use of sedatives or neuromuscular blockers. In these patients, the self-evaluation of pain is not viable, and other instruments must be used. In this regard, a number of validated scales are currently available.9–14 The systemic use of these scales has been shown to improve pain management, with a lesser need for sedating analgesics, and better clinical outcomes.15,16 However, in patients subjected to deep sedation or neuromuscular block, pain is not easy to evaluate. The monitoring of different vital signs has therefore been proposed, such as arterial pressure and heart rate (HR), for evaluating pain. The results obtained by the different studies are contradictory,17,18 however, and this approach is therefore presently not recommended.1,2
The bispectral index (BIS) has recently been proposed as an objective method for evaluating pain in non-communicative patients. This parameter is derived from the electroencephalographic (EEG) tracing, and reflects brain reactivity.19 Some studies have found the BIS to fluctuate in response to pain, even in deeply sedated patients–thus supporting its potential usefulness for the detection of pain in non-communicative patients.20
There has been only limited research on pain during nursing procedures in sedated critical patients, and the usefulness of vital signs and of the BIS as indicators of pain has not been well established. Considering the above, the present study was carried out with the following objectives: (1) to evaluate the prevalence of pain in the course of two common nursing procedures; and (2) to evaluate the usefulness of vital signs and of the BIS in detecting pain during such procedures.
Patients and methodsA prospective, repeated-measures analytical observational study was carried out in a series of medical-surgical patients. The study was conducted between September 2010 and April 2011 in the DICM of Santa Creu i Sant Pau Hospital in Barcelona (Spain), and was approved by the Clinical Research Ethics Committee of the hospital, with adherence to the ethical principles of the Declaration of Helsinki (2013).21 Since the patients were unable to communicate, a member of the research team obtained written informed consent to participation from their legal representatives.
PatientsThe following inclusion criteria were established: (1) patients over 18 years of age; (2) admission to the DICM; (3) a need for mechanical ventilation and pharmacological sedation; and (4) a need for endotracheal aspiration and/or mobilization with turning.
The following exclusion criteria were established: (1) patients with acute brain damage; (2) confirmed cognitive defects or decompensated psychiatric disease; (3) treatment with neuromuscular blockers; (4) limitation of therapeutic effort or brain death; and (5) deep sedation (Richmond Agitation Sedation Scale [RASS] score −5).22
ProceduresThe two procedures evaluated were endotracheal aspiration and mobilization with turning. The choice of these procedures was based on the results of earlier studies,7,9 which showed them to be potentially painful for patients.
Variables and instrumentsThe presence of pain was evaluated using the Behavioral Pain Scale (BPS)9 (Table 1), which contemplates three behavioral indicators: facial expression, movement of the upper extremities, and adaptation to mechanical ventilation. Each indicator is scored from 1 to 4, and the total score ranges from 3 (absence of pain) to 12 (maximum pain). A BPS score of >3 indicates pain, and a BPS score of ≥5 indicates significant pain.23
Behavioral Pain Scale.
| Facial expression | |
| Relaxed | 1 |
| Partially tightened | 2 |
| Fully tightened | 3 |
| Grimacing | 4 |
| Movements of the upper extremities | |
| No movement | 1 |
| Partially bent | 2 |
| Fully bent | 3 |
| Permanently retracted | 4 |
| Adaptation to mechanical ventilation | |
| Adapted movements | 1 |
| Good adaptation most of the time | 2 |
| Struggling with respirator | 3 |
| Impossible to ventilate | 4 |
Presence of pain with BPS >3. Presence of significant pain with BPS ≥5.
The following vital signs were evaluated: systolic blood pressure (SBP), mean blood pressure (MBP), heart rate (HR) and respiratory frequency (RF). These signs were obtained through continuous monitoring at the patient bedside (General Electric MD 15T®, Finland; General Electric Company, Solar TM 8000M/i, Spain), with recordings once every minute.
The BIS is a noninvasive monitoring tool that measures different cortical electrical parameters by means of electrodes positioned on the forehead of the patient. The index can range from 0 (total suppression of the EEG tracing) to 100 (fully awake), according to the level of consciousness of the patient. Specifically, a BIS of 90–100 is correlated to a good waking state, while an index of 70–80 indicates mild sedation, 60–70 reflects moderate sedation, and 30–60 corresponds to deep sedation similar to that observed during general anesthesia.19 The BIS numerical values were obtained using a BIS VISTA™ monitor (Aspect Medical Systems Inc., Newton, MA, USA), which converts the data into numerical values at 5-s intervals.
The level of sedation was evaluated using the RASS,22 which has been validated for measuring the depth of sedation and agitation in adult patients subjected to mechanical ventilation. The RASS score ranges from −5 (patients unresponsive to stimuli) to +4 (combative patients).
ProtocolPatient inclusion was made conditioned to the availability of the principal investigator (PI). All the evaluations were made by the PI of the study–a nurse previously trained in the use of the BPS in over 100 patients. The nurses in charge of patient care carried out the procedures in accordance with the needs of the patient and following the interventional protocols of the DICM. In certain cases, and depending on the clinical condition of the patients, analgesia and sedation were provided before carrying out the procedures.
A maximum of four procedures per patient were evaluated, establishing a minimum period of 30min between two successive evaluable procedures carried out in the same patient.
The patients were evaluated at three timepoints. A resting baseline evaluation was made at least 30min before starting the nursing procedure (T0); a second evaluation was made 5min before starting the procedure (pre-procedure, T1); and a third evaluation was made during the procedure (T2).
The PI recorded the exact time at which the evaluation corresponding to each timepoint was made.
At T0 the demographic data (age, gender) and variables related to treatment were recorded–including the level of sedation (RASS) and the analgesic and sedating drugs administered in continuous perfusion and/or as intermittent bolus doses during the four hours before data collection. This period was considered to correspond to the mean elimination half-life of the drugs included in the analgesia and sedation protocol of the DICM. The PI prepared the skin of the forehead of the patient with isopropyl alcohol and positioned the BIS sensors according to the instructions of the manufacturer. After checking the impedance of the electrodes and confirming good signal quality, the BIS monitor was turned on to compile the data.
For evaluating pain based on the BPS, the patient was previously observed by the PI for one minute at T0 and T1, and pain assessment was then made at T2 during the procedure.
At the end of the procedure, the means of the absolute values corresponding to systolic blood pressure, mean blood pressure, HR and RF were calculated from the continuous monitoring data obtained, and the BIS information was entered in electronic format. The BIS data were selected from the registry of the evaluation time, calculating a delay of one minute between the point of stimulation and the BIS value.
Data analysisThe normality of the distribution of the variables was confirmed using the Kolmogorov–Smirnov test.
The categorical variables (gender, diagnosis, type of analgesia and sedation, and preventive analgesia and sedation) were expressed as percentages and number of cases. The quantitative variables (BPS score, systolic blood pressure, mean blood pressure, HR, RF and BIS) were expressed as medians and interquartile range (IQR1-IQR3).
In order to determine whether the existence of pain can be predicted from the observation of pain behavior and the physiological indicators, comparisons were made of the BPS scores, the absolute values of the vital signs and the BIS values before (T1) and during (T2) the procedures, using the Mann–Whitney U-test.
The effect of pain present before the procedures upon pain during the procedures was evaluated by creating a new variable: the mean difference in the BPS scores between T1 and T2. The values were expressed as the median and IQR.
The clinical relevance of the differences was assessed by analyzing the variations in vital signs and BIS values as percentage changes. The data were reported as the median and IQR. In accordance with the results of earlier studies,24 we a priori defined clinical relevance as corresponding to a percentage change of ≥10%.
Comparison of the vital signs and BIS values between T1 and T2 was carried out using the Wilcoxon test.
Lastly, a subgroups analysis was used to compare the effects of administration or non-administration of preventive analgesia and sedation. Specifically, comparisons were made of the BPS scores and the percentage changes in BIS between the patients who had received preventive analgesia and sedation and those who had not received such treatment, based on the Mann–Whitney U-test.
A two-tailed approach was used, establishing a level of statistical significance of 5% (α=0.05). The SPSS® version 21.0 statistical package was used throughout.
ResultsBaseline characteristics of the patientsThe baseline characteristics of the patients are shown in Table 2. A total of 146 procedures (84 endotracheal aspirations and 62 mobilizations) were evaluated in 70 patients. There were no statistically significant differences between endotracheal aspiration and mobilization. The mean duration of the aspiration procedure was 8s, while the mean duration of mobilization was four minutes.
Baseline characteristics of the study population (n=70).
| Age in years, median (IQR) | 71 (62–79) |
| Gender, n (%) | |
| Females | 25 (36) |
| Males | 45 (64) |
| Reason for admission, n (%) | |
| Medical | 7 (10) |
| Surgical | 63 (90) |
| BPS score, n (%) | |
| =3 | 27 (39) |
| >3 | 43 (61) |
| ≥5 | 23 (33) |
| RASS score, n (%) | |
| ≥+1 | 11 (15) |
| 0 to −2 | 22 (32) |
| −3 to −4 | 37 (53) |
| BIS, median (IQR) | 62 (50–72) |
| Analgesia, n (%) | |
| Without analgesia | 4 (6) |
| Morphine cp | 42 (60) |
| Remifentanil cp | 3 (4) |
| Bolus dose analgesia | 11 (16) |
| Paracetamol or NSAIDs | 14 (20) |
| Others | 4 (6) |
| Sedation, n (%) | |
| Propofol cp | 37 (53) |
| Midazolam cp | 31 (44) |
| Bolus dose sedation | 28 (40) |
| Combination of several drugs | 2 (3) |
NSAIDs: nonsteroidal antiinflammatory drugs; BIS: bispectral index; BPS: Behavioral Pain Scale; cp: continuous perfusion; RASS: Richmond Agitation Sedation Scale; IQR: interquartile range.
Sixty-one percent of the patients suffered pain under resting conditions (T0), with a median BPS score of 4 (IQR: 3–5). Thirty-three percent of the patients presented significant pain (BPS≥5).
Pain during the proceduresPain behavior was noted in 94% of the procedures evaluated, with a median BPS score of 6 (IQR: 5–8). In 86% of the procedures, the pain was scored as significant (BPS≥5). There were no significant differences in BPS score between mobilization with turning and endotracheal aspiration (6 [5–8] vs. 7 [6–8]; p=0.146, respectively).
The comparisons of the pain scores before (T1) and during (T2) the procedures are shown in Fig. 1. Both the global comparisons (4 [3–5] vs. 6 [5–8]; p<0.001, respectively) and the partial comparisons referred to facial expression (2 [1–2] vs. 2 [2–3]; p<0.001, respectively), movement of the extremities (1 [1–2] vs. 2 [2–2]; p<0.001, respectively) and adaptation to mechanical ventilation (1 [1–2] vs. 2 [2–3]; p<0.001, respectively) were statistically significant.
The patients with pain (BPS>3) under resting conditions (T0) experienced more pain during the procedures (T2) than those without resting pain (BPS=3) (7 [6–8] vs. 6 [5–8]; p=0.012, respectively).
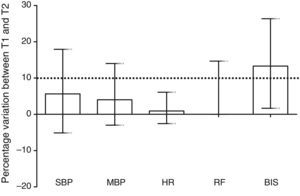
Vital signs and bispectral index during the proceduresThe vital signs (systolic blood pressure, mean blood pressure, HR and RF) and the BIS increased significantly from T1 to T2 (108 [94–121] vs. 118 [102–132]; p<0.001, 73 [62–80] vs. 76 [67–85]; p<0.001, 88 [76–108] vs. 90 [80–108]; p=0.002, 16 [12–20] vs. 17 [13–22]; p<0.001, 58.5 [47–72] vs. 71 [59–80]; p<0.001, respectively). However, the percentage change was only clinically relevant (≥10%) for the BIS values (13% [IQR: 2–26%]) (Fig. 2). The variation in BIS was ≥10% in 72% of the pain behavior observations.
Percentage variation of the different vital signs and BIS between the pre-procedure timepoint (T1) and the procedure (T2). The broken line marks 10%, which is the value a priori considered to be clinically relevant. Only the BIS values were clinically relevant. Values expressed as the median and interquartile range. BIS: bispectral index; HR: heart rate; RF: respiratory frequency; MBP: mean blood pressure; SBP: systolic blood pressure.
Before the procedures, and based on the criterion of the nurse and/or physician in charge, preventive analgesia was administered in 7% of the procedures and preventive sedation in 21% (Table 3).
Effects of preventive analgesia and sedation upon pain and the bispectral index.
| Analgesia n=10 (7%) | Without analgesia n=136 (93%) | p-value | |
|---|---|---|---|
| Baseline BPS | 5 (3–6) | 4 (3–5) | 0.179 |
| Pre-procedure BPS (T1) | 7 (5–9) | 4 (3–5) | 0.001 |
| Procedure BPS (T2) | 4 (4–6) | 6 (6–8) | <0.001 |
| T1–T2 difference | −2 ([−5]–0) | 3 (1–4) | <0.001 |
| % variation BIS T1–T2 | 5 ([−40]–18) | 16 (3–37) | 0.021 |
| Sedation n=31 (21%) | Without sedation n=115 (79%) | p-value | |
|---|---|---|---|
| Baseline BPS | 4 (3–5) | 4 (3–5) | 0.086 |
| Pre-procedure BPS (T1) | 5 (4–7) | 4 (3–5) | <0.001 |
| Procedure BPS (T2) | 6 (4–7) | 6 (6–8) | <0.82 |
| T1–T2 difference | 1 ([−3]–3) | 3 (1–4) | 0.001 |
| % variation BIS T1–T2 | −5 ([−40]–7) | 20 (9–37) | <0.001 |
BPS: Behavioral Pain Scale.
Values expressed as the median (interquartile range).
With regard to analgesia, the patients who received a preventive analgesic bolus dose before the procedures showed a significant decrease in pain between T1 and T2 versus those who did not receive preventive analgesia (−2 [IQR: {−5}–0] vs. 3 [IQR: 1–4]; p<0.01, respectively).
Likewise, the patients who received a preventive analgesic bolus dose before the procedures showed a statistically smaller and clinically non-relevant change in BIS versus those who did not receive preventive analgesia (5% [IQR: {−40}–18%] vs. 16% [IQR: 3–37%]; p=0.021, respectively).
With regard to sedation, the patients who received an additional sedation dose before the procedures experienced an increase in pain between T1 and T2, though the increase was smaller than in those who did not receive preventive sedation (1 [IQR: {−3}–3] vs. 3 [IQR: 1–4]; p<0.001, respectively).
Likewise, the patients who received an additional sedation bolus dose before the procedures also presented a statistically smaller and clinically non-relevant change in BIS versus those who did not receive sedation (−5% [IQR: {−40}–7%]) vs. 20% [IQR: 9–37%]; p<0.001, respectively.
DiscussionThe main result of our study can be summarized as follows: (1) the patients in our DICM suffer resting pain; (2) mobilization with turning and endotracheal aspiration are painful procedures; (3) the physiological signs are not useful for evaluating pain; (4) the variation in BIS could be useful for evaluating pain; and (5) preventive analgesia may decrease pain during the procedures.
Resting painIn our series, 61% of the patients experienced pain (BPS>3) under resting conditions, and 33% suffered significant pain (BPS≥5). This high percentage is not surprising and is consistent with the data found in the literature on the prevalence of resting pain in critical patients who are unable to communicate. Chanques et al., in a series of surgical cases,15 found 63% of their patients to have significant pain under resting conditions. This figure dropped to 42% following a training initiative targeted to nurses and physicians, in which improvements were made in the detection of pain and the administration of analgesic treatment. Other studies have shown the objective control of analgesia, sedation and delirium to improve detection and treatment of the problem.25
Although these scales are simple to apply, they are little used in routine clinical practice,23 and the incidence of resting pain remains high. The studies published to date show important discrepancies between actual clinical practice and the current recommendations.1,2 On the other hand, we should ask ourselves whether health professionals are well instructed on how to assess pain behavior. In a recent study,26 the authors evaluated interobserver reliability of the BPS scale under resting conditions and during a painful procedure. The facial expression subscale was seen to show poor concordance and low correlation. These results reflect a need for sufficient prior training and a minimum level of experience in order to guarantee adequate pain evaluation through behavioral indicators.
This approach therefore could be useful in developing appropriate educational programs and future guidelines for the management of sedation and analgesia in the DICM. Emphasis should be placed on the need to evaluate pain using the validated scales at our disposal, in order to identify and treat the problem correctly.9–14
Pain during the nursing proceduresCritical patients undergo multiple diagnostic and therapeutic procedures carried out by nurses, and most of them describe having experienced pain during the procedures even several years later.27 Our results indicate that the procedures we have studied are painful for most patients. The percentages obtained are consistent with the results recently published by the Europain® study.28 The authors evaluated pain in 3850 conscious patients in 192 Intensive Care Units from 28 countries. The results showed a significant increase in pain from the start to the time of performing the 12 procedures evaluated–including mobilization and endotracheal aspiration. Furthermore, the study found pre-procedure pain to be a risk factor for greater pain intensity during the procedures. The authors concluded that good control of resting pain can lessen pain during the procedures.
Usefulness of vital signs and the bispectral index in the evaluation of painIn patients unable to communicate with the health professionals, several vital signs have been postulated for evaluating pain. However, vital signs are not specific of pain and can be influenced by the administration of drugs (e.g., vasopressors, betablockers, antiarrhythmic agents) or the underlying disease condition itself (sepsis). In fact, several studies have shown that these parameters increase during both painful and non-painful procedures,29 and/or remain without change during procedures shown to be painful by validated scales.30 Our results reveal significant changes in all the vital signs and in the BIS values, though only the latter were clinically relevant. Our findings therefore reinforce the evidence suggesting that vital signs should not be used isolatedly for assessing pain behavior in patients who are unable to communicate verbally.1,2
The BIS has been used to monitor levels of consciousness in patients under sedation and anesthesia.19 Earlier studies in critical patients have shown that transient increments of between 5 and 20% in the BIS values can be associated to pain.17,18 However, multiple factors (e.g., tactile or hearing stimuli) can interfere with these variations. Some authors support the idea the BIS could be useful provided these factors are adequately controlled.18 In any case, our results coincide with those already found in the literature, and support the idea that variations in BIS can be useful for the evaluation of pain–though further studies are needed to confirm this possibility.
Additional analgesics and sedatives before the proceduresMost patients admitted to the DICM receive some kind of analgesic treatment. According to a French study,23 on the second day of admission 72% of the patients were receiving some analgesic medication. On day four this percentage was found to be 55%, versus 50% on day 6 of admission. In our series, practically all patients received some type of analgesia. However, the administered medication doses do not seem to suffice to alleviate resting pain, and are clearly insufficient in avoiding pain during the nursing procedures.
For this reason, preventive analgesia before performing a procedure could be a good strategy. In our series, the nurse or physician decided to provide preventive analgesia in only 7% of the procedures. Such limited use of preventive analgesia in our setting is consistent with the different multicenter and multinational observational studies found in the literature.7,28
To our knowledge, the efficacy of preventive analgesia has only been evaluated in three procedures: femoral catheter removal,31 the aspiration of secretions,32 and chest drain removal.33–36 The results of these studies are moreover inconclusive.
Fulton et al.31 evaluated the efficacy of morphine, fentanyl, subcutaneous lidocaine or placebo administered before femoral artery catheter removal in 130 patients subjected to cardiac catheterization. They recorded no differences in relation to pain perception. The authors concluded that the procedure was not sufficiently painful for preventive analgesia to be able to demonstrate its benefits.
Brocas et al.32 evaluated the effect of the preventive administration of alfentanyl before endotracheal tube aspiration upon the BIS value in 10 critical patients subjected to mechanical ventilation. The BIS increased significantly in aspiration performed without preventive analgesia versus aspiration performed after preventive alfentanyl administration. The authors concluded that preventive analgesia was effective in reducing pain evaluated by the BIS.
Puntillo and Ley33 evaluated the efficacy of morphine, ketorolac or patient information on the procedure before chest drain removal in 75 heart surgery patients. These authors likewise found no differences between the groups in relation to the perception of pain, and also concluded that the process was probably not painful enough for preventive analgesia to be able to demonstrate its benefits. However, in other studies, significantly lower pain scores were recorded in patients who before chest drain removal had received intravenous morphine plus relaxation exercises34, sufentanil or fentanyl35 or topical valdecoxib.36
It is easy to imagine that patients admitted to the DICM would wish to have pain treated on a preventive basis with drugs or other means before undergoing painful procedures. Consequently, preventive analgesia and/or non-pharmacological interventions are currently recommended for alleviating pain in adult patients before chest drain removal is carried out, and similar measures are also advised in other potentially painful procedures.1 On the other hand, it must be taken into account that the administration of analgesic medication–mainly opioids and nonsteroidal antiinflammatory drugs–can produce side effects.
On the basis of the above, different authors have proposed the concept of dynamic analgesia, which could allow a lowering of the analgesia dose under resting conditions and an increase before potentially painful procedures are performed. The idea would be similar to that used for avoiding the accumulation of sedative agents. Strategies such as “sequential sedation”, “dynamic sedation” or “daily sedation interruption” have demonstrated their efficacy in preventing the complications associated to prolonged sedation.1,2
Regarding sedating drug use before the procedures, our results show that it is not as effective as analgesia in avoiding pain. In this regard, pain can cause agitation or restlessness in the critical patient, and its management should be based on analgesia rather than on sedation.
Study limitationsOur study has a number of limitations. Firstly, it is a single-center study in sedated patients subjected to mechanical ventilation and mostly subjected to surgery. As a result, the findings cannot be extrapolated to other types of patients. Secondly, no non-painful procedure was used as control. In this regard, a control group would have helped to discriminate between the effects inherent to the procedure and the simple effect of interacting with the patient. On the other hand, evaluation after completing the procedures was not made, but would have helped clarify the evolution of pain associated to the procedures. Finally, the number of patients who received preventive analgesia was small; as a result, we are unable to draw firm conclusions on these partial results.
ConclusionsCritical patients who are unable to communicate continue to experience resting pain. Furthermore, mobilization with turning and endotracheal aspiration are both painful procedures. The detection and treatment of baseline pain, enhanced by routine maneuvers, confirms the usefulness of the clinical scales and advises the administration of preventive analgesia and the expanded use of the BIS.
Financial supportThis study has received no financial support.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to Kathleen Puntillo, RN, PhD, FAAN, FCCM, professor emeritus and senior investigator of the Scientific Physiological Nursing Department of the University of California at San Francisco (UCSF), for her valuable comments on this article.
Please cite this article as: Robleda G, Roche-Campo F, Membrilla-Martínez L, Fernández-Lucio A, Villamor-Vázquez M, Merten A, et al. Evaluación del dolor durante la movilización y la aspiración endotraqueal en pacientes críticos. Med Intensiva. 2016;40:96–104.