Severe traumatic brain injury (sTBI) remains prevalent in the young adult population. Indeed, far from descending, the incidence of sTBI remains high. One of the key bases of treatment is to avoid, detect and correct secondary injuries of systemic origin, which aggravate the primary lesion. Much of this can be achieved by maintaining an adequate physiological microenvironment allowing recovery of the damaged brain tissue. General care measures are nonspecific actions designed to meet that objective. The available guidelines on the management of sTBI have not included the topics contemplated in this consensus. In this regard, a group of members of the Latin American Brain Injury Consortium (LABIC), involved in the different aspects of the acute management of sTBI (neurosurgeons, intensivists, anesthesiologists, neurologists, nurses and physiotherapists) were gathered. An exhaustive literature search was made of selected topics in the Lilacs, PubMed, Embase, Scopus, Cochrane Controlled Register of Trials and Web of Science databases. To establish recommendations or suggestions with their respective strength or weakness, the GRADE methodology (Grading of Recommendations, Assessment, Development and Evaluation) was applied. Additionally, certain recommendations (included in complementary material) were not assessed by GRADE, because they constitute a set of therapeutic actions of effective compliance, in which it was not possible to apply the said methodology. Thirty-two recommendations were established, 16 strong and 16 weak, with their respective levels of evidence. This consensus attempts to standardize and establish basic general care measures in this particular patient population.
El Traumatismo craneoencefálico grave (TCEg) continúa siendo prevalente en la población adulta joven. Lejos de descender, su incidencia se mantiene elevada. Uno de los pilares en los que se asienta su tratamiento es evitar, detectar y corregir complicaciones secundarias de origen sistémico que agravan la lesión primaria. Gran parte de este objetivo se logra manteniendo un microambiente fisiológico adecuado que permita la recuperación del tejido cerebral lesionado. Las medidas de cuidados generales son acciones inespecíficas destinadas a cumplir dicho objetivo. Las guías disponibles de manejo del TCEg no han incluido la mayoría de los tópicos motivo de este consenso. Para ello, hemos reunido un grupo de profesionales miembros del consorcio latinoamericano de lesión cerebral (LABIC), involucrados en los diferentes aspectos del manejo agudo del TCEg (neurocirujanos, intensivistas, anestesiólogos, neurólogos, enfermeros, fisioterapeutas). Se efectuó una búsqueda bibliográfica en las bases de datos Lilacs, Pubmed, Embasse, Scopus, Cochrane Controlled Register of Trials y Web of Science de los tópicos seleccionados. Para establecer recomendaciones o sugerencias con su respectiva fortaleza o debilidad, fue aplicada la metodología GRADE (Grading of Recommendations, Assessment, Development and Evaluation). Adicionalmente, ciertas recomendaciones (incluidas en material complementario) no fueron valoradas por GRADE, por ser las mismas un conjunto de acciones terapéuticas de cumplimento efectivo, en las que no fue posible aplicar dicha metodología. Fueron establecidas 32 recomendaciones; 16 fuertes y 16 débiles, con su respectivo nivel de evidencia. El presente consenso intenta homogeneizar y establecer medidas de cuidados generales básicas en esta población de individuos.
Traumatic brain injury (TBI) is the silent epidemic of our time (TBI).1 In Latin America, where we do not have reliable official data, it affects young male adults predominantly and it is often the result of car crashes or violence.2,3 Mortality rate is higher compared to developed countries and its prevalence grows on a daily basis.2,3 Conversely, the epidemiologic profile in developed countries is different; mortality is lower, here predominantly the cause is sports traumas, and prevalence has dropped significantly.4 TBI is a dynamic, progressive, and heterogeneous entity.5 From the standpoint of its mechanism of production, 2 are the most significant ones: focal, due to contact damage, and diffuse, that develops as a consequence of phenomena of acceleration/deceleration sustained by the cerebral parenchyma.5,6 Its pathophysiology is characterized by the primary lesion that occurs when the trauma is sustained. It is irreversible, there is no specific therapy to treat it, and secondary lesions are represented by different systemic or intracranial pathological processes that originated when the primary lesion occurred.5,6 Secondary lesions are characterized by being reversible, preventable, and treatable. At the moment, secondary lesions are at the foundation on which the therapeutics of TBI stands.5,6 A third mechanism of lesion production is the so-called tertiary damage. It is the product of the complications that can occur during the management of the patient such as infections or damage due to the therapeutics used.7 At the end of the 1990s, the Brain Trauma Foundation (BTF) published the first evidence-based recommendations as a guide for the optimal management of TBI. These recommendations have been updated periodically and now they are in their fourth edition.8–10 All of them have been renewed and refined across time and their content has focused mainly on who is eligible to be treated of a TBI; the importance of avoiding secondary factors of the lesion such as hypotension or hypoxemia, what the best time is to monitor intracranial pressure (ICP), and how the management of endocranial hypertension should be done.8–10 Additionally, they recommend other aspects for the management of nutrition, seizure prophylaxis, infections, and deep venous thrombosis.8–10 There is no doubt that in the management of TBI, advanced and integrated multimodal neuromonitoring plays an important role here;6 however, in most parts of the world, dominated by centers with scarce economic resources, access to basic neuromonitoring systems such as measuring ICP is not an easy thing to do.2,3 Yet despite these differences, the centers that have many resources and those that have scarce resources share something in common: general clinical care. Thus, the general measures achieved in this consensus are applicable to any healthcare setting regardless of the level of resources available. Encouraged by it, the main objective of this consensus is to establish recommendations or suggestions destined to homogenize and highlight the comprehensive and relevant role that the different measures of general care play in the management of victims of TBI.
Consensus methodologyDefinition of general care measuresThere is no universal or validated definition. As a consequence, we developed the following one: «General care measures are all those common and non-specific actions aimed at the routine care of individuals who have sustained a TBI in order to avoid lesions or secondary, tertiary complications with the ultimate goal of contributing to improve the quality of final outcomes».
Building up the working groupWhile writing the consensus document we followed the criteria established by the Glaser method based on an update of the «state of the art» of different aspects including general care.11–14 Basically, consensus was achieved by a coordinating group, predominantly neurointensivists, within the Latin American Brain Injury Consortium (LABIC) with over 15 year experience in the management of TBI Additionally, previous participation in other consensus documents and training in medical reference search in the following databases were prerequisites to be included in the working group: LILACS, PubMed, Embasse, Scopus, Cochrane Controlled Register of Trials, and Web of Science, as well as having published, at least, 5 research papers. The remaining members of the working group were doctors specialized in neurocritical care, neurologists, neurosurgeons, nurses, and physical therapists, also LABIC members, with, at least, a 10-year experience and savvy on reference search in the aforementioned databases. The aforementioned criteria were followed, and a multidisciplinary consensus group was built including 18 professionals from 7 different Latin American countries: Argentina, Brazil, Bolivia, Colombia, Cuba, Chile, and Ecuador.
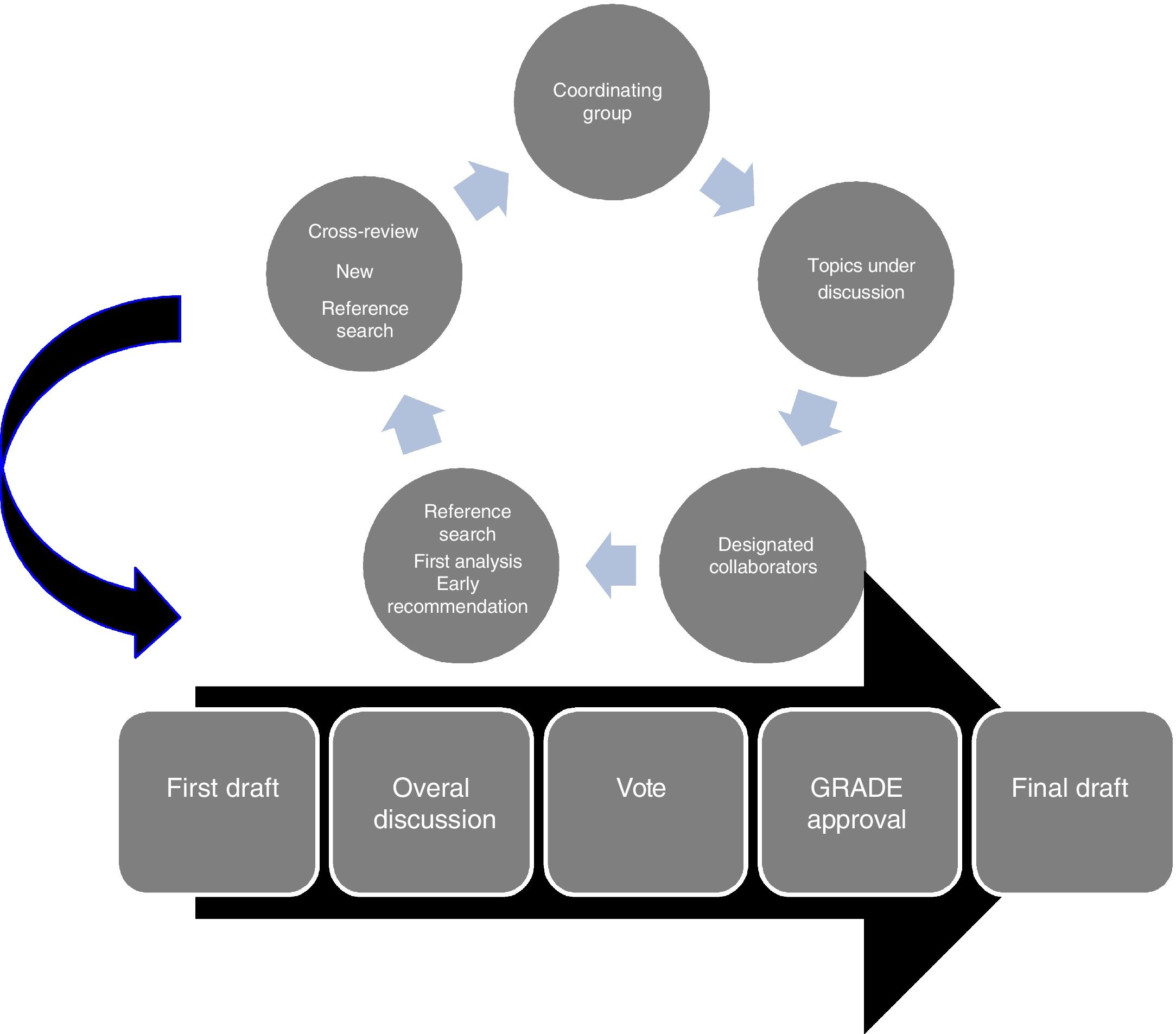
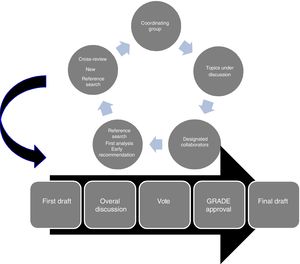
Achieving consensusThe first discussion meeting where consensus criteria were established was held in Quito, Ecuador back in November 2017 where the coordinating group defined the strategy to follow as shown on Fig. 1. The topics of interest to be included that needed to meet to definition of general care were analyzed. Similarly, to be included in the consensus document they should not be part of the current guidelines on the management of TBI.10 We should mention here that 2 topics (mechanical ventilation and sedoanalgesia) are barely discussed in the aforementioned guidelines without recommendations or suggestions on how to carry out these measures Fig. 2.
Participants were divided into groups of 2–3 members depending on their field of expertise and levels of experience. Questions for each topic were proposed. Each group was in charge of a relevant and updated reference search of the topic under discussion. The studies were extensively reviewed to establish the best current research evidence available to be able to recommend a specific procedure.15 The best actual research evidence available was defined based on the efficacy and safety of the measure under discussion. Also, evidence was considered as a new evidence on a certain topic when it overruled previously accepted regimens and replaced them for other new ones.16 Evidence included quantitative and qualitative assessments according to their correlation with the methods of research, consistency of results, discussion, and conclusion.16
Reference searchIn order to achieve consensus, a comprehensive reference search was conducted in the following databases: Cochrane Central Register of Controlled Trials (CENTRAL), Medline, Embase, LILACS, Scopus, Ovid, and Web of Science. Afterwards, the reference lists of all the review papers, meta-analyses, systematic reviews, and primary studies available were analyzed. We should mention that the difference searches used different keywords depending on the questions asked. Regarding limits, the searches focused on papers written in Spanish and English since 1990 until the present time and in the adult population only.
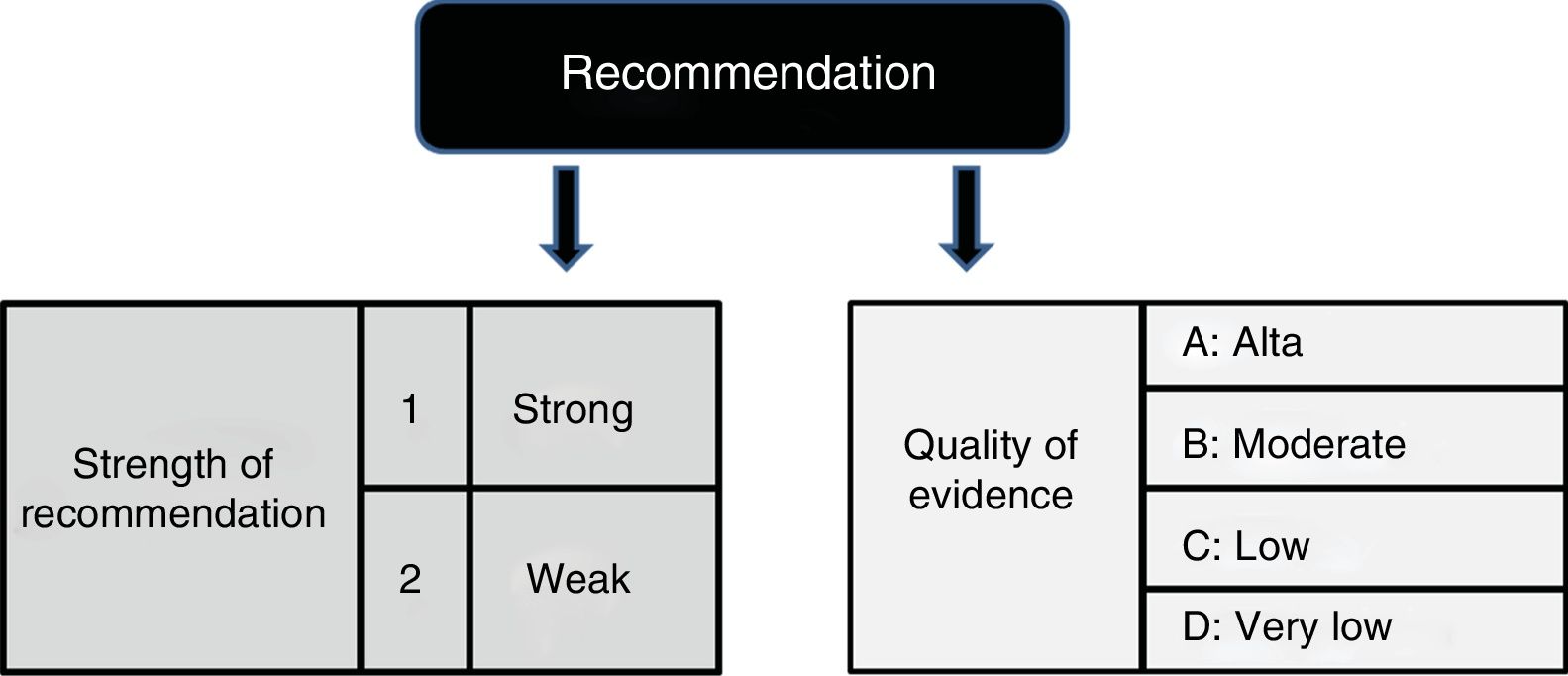
Degree of recommendationsIn all the questions included in the consensus documents, the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology to assess the evidence available was used.17 The criteria used to select the evidence was based on the population, the intervention, the comparator, the elements of the results gvien to the standardized query, and the study design.17
After a qualitative analysis of the medical literature, the GRADE methodology was used to determine the quality of the evidence available, that is, to assess the confidence needed to analyze the effect of the quantitative intervention and the level of recommendation.17 We should mention that when systematic reviews that responded to some of the questions posed by the guidelines were identified, we assessed their quality based on the tool used for assessment purposes.18
All recommendations were binary and categorized as strong or weak:
- -
Strong recommendation: we do recommend or do not recommend.
- -
Weak recommendation: we do suggest or do not suggest.
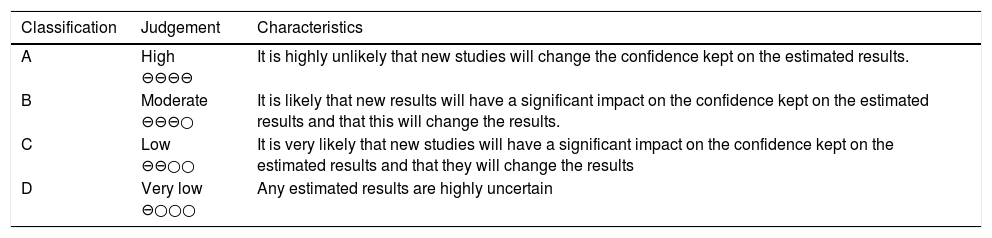
According to the GRADE methodology, the strength of a recommendation is defined based on how sure we can be that the wanted effects of a measure exceed its unwanted effects.17 When establishing the strength of a recommendation, the panel considered the balance between the wanted and unwanted consequences, the quality of evidence, the implication of the resources available, and the patients’ average values and preferences for different results and options of management. Also, the quality of the evidence available was assessed and classified as high moderate or low (including very low) (Table 1).17
Overall quality of the GRADE evidence.
| Classification | Judgement | Characteristics |
|---|---|---|
| A | High ⊖⊖⊖⊖ | It is highly unlikely that new studies will change the confidence kept on the estimated results. |
| B | Moderate ⊖⊖⊖○ | It is likely that new results will have a significant impact on the confidence kept on the estimated results and that this will change the results. |
| C | Low ⊖⊖○○ | It is very likely that new studies will have a significant impact on the confidence kept on the estimated results and that they will change the results |
| D | Very low ⊖○○○ | Any estimated results are highly uncertain |
| Strength of recommendation | Clinical implications | |
|---|---|---|
| Strong | «We do recommend» | Most individuals should receive the recommendation. |
| Weak | «We do suggest» | Recognition that there may be other options available. Decisions are left to the discretion of the treating physician while observing the patients’ possible preferences. |
We should mention that some of the recommendations included in the supplementary data were not assessed using the GRADE methodology because they were a set of recommendations for effective compliance that could not be assessed using this methodology. After taking these steps, a very first draft of 5 sections was written: 1) clinical question; 2) recommendation; 3) grounds; 4) evidence summary, 5) back up references.
When this stage was over, every item was cross reviewed by a different group of the writing team that proceeded to review the topic anonymously. The coordinating group directed this task of exchanging suggestions and corrections together with the authors through the e-mail and simultaneous videoconferences using Skype or Zoom. When the results of these phases became available, the coordinating group prepared a second draft that was itemized in all of its aspects by all the authors responsible for the consensus document. When this stage was over, anonymous votes were cast electronically to assess the degree of consensus. Eighty per cent agreement was required to participants to achieve approval. The final draft was discussed once again, analyzed in-depth, and eventually submitted to an external review committee that included renown colleagues who were also experts on the issue at stake. The suggestions, criticism, and recommendations made by this committee were taken into consideration prior to the submission of the final draft for publication. As other guidelines already point out and based on the low levels of evidence identified, the treatment recommendations are not representative of the standard of care but summarize the best current clinical practice.19
Topics under discussionThe questions asked regarding the items under discussion tried to cover the entire spectrum of a set of general measures (according to the definition established) often used for the general management of patients with TBI.
The following aspects are included in the consensus documents, which were divided into 3 large groups:
- a
General care:
- 1
Position of the head.
- 2
Use of cervical spine immobilization.
- 3
Mouth hygiene.
- 4
Management of artificial airways.
- 5
Eye protection.
- 1
- b
Physiological homeostasis:
- 1
Selection of resuscitation flow.
- 2
Optimization of systemic arterial pressure.
- 3
Management of body temperature.
- 4
Maintenance and monitoring of glycemia levels.
- 5
Desired concentration of hemoglobin.
- 6
Management of serum sodium.
- 7
Management of sedation and analgesia.
- 8
Ventilation and oxygenation.
- 9
Prevention of stress ulceration and upper gastrointestinal bleeding.
- 10
Nutritional aspects.
- 1
- c
Supplementary data (measures where the GRADE methodology could not be implemented).
- 1
Maintenance and management of venous accesses, cannulas, drainages, and monitoring systems.
- 2
Management of catheters for IPC and tissue oxygen pressure (PtiO2) monitoring.
- 3
Prevention of pressure ulcers.
- 4
Mobilization and physical therapy in the acute phase.
- 5
Aspects associated with the management of the digestive tube (gastroparesis, diarrhea, constipation).
- 6
Strategies to control infections.
- 1
The main objective of this document is to serve as an update of the best evidence available on general care measures in the acute phase during the management of TBI. Reference search included randomized clinical trials, systematic reviews, meta-analyses, and clinical practice guidelines of the aforementioned databases. Based on the results obtained from the reference analysis and after applying the GRADE methodology, we established recommendations that were graded according to their level of evidence and the degree of strength. Eventually, we developed 32 fin. l recommendations as shown on Table 2. Additionally, we highlighted certain recommendations and patterns of care and general management of TBI where the GRADE methodology could not be applied for the reasons already mentioned, which is why they are not part of the main body of the manuscript, but still remain available as supplementary data
General care for the management of TBI: consensus recommendations.
| Topic | Recommendation | Strength | Level of evidence | Reference (annex) |
|---|---|---|---|---|
| General care | ||||
| Position of the head | We suggest resting the head in a 30° angle from the horizontal plane and in a neutral position (not extended or flexed) in order to minimize ICP. | Weak | Low | 5,10, 20−33 |
| Use of cervical spine immobilization | We suggest cervical spine immobilization until additional tests are performed to confirm or discard spinal lesions. | Weak | Low | 34−46 |
| Mouth hygiene | We suggest oral periodic hygiene with chlorhexidine to reduce the incidence of associated pneumonia. | Weak | High | 47−51 |
| Management of artificial airways | a. Monitorization of the pressure of the endotracheal tube balloon. | Strong | Low | 52−56 |
| We recommend the routine control of inflation and pressure of the endotracheal tube balloon (20 cm–30 cm of H2O) to avoid tracheal ischemic lesions and micro-aspirations. | ||||
| b. Management of respiratory secretions. | Strong | Low | 57−61 | |
| We recommend the aspiration of secretions through the endotracheal tube only when necessary to maintain the airways patency. | ||||
| c. We do not recommend a system in favor of another to eliminate bronchial secretions and avoid MVAP. We do recommend using a closed system in favor of the open system in patients in whom it is required to preserve the end-expiratory lung volume. | Strong | Low | 62−65 | |
| Eye protection | We recommend routine eye monitoring and care to see any possible lesions on the surface of the eye. | Strong | Low | 66−70 |
| Physiologic homeostasis | ||||
| Fluid therapy | a. During the early stages of resuscitation and maintenance we recommend using a physiological saline solution on the colloids to restore and maintain a proper intravascular volume and CPP | Strong | Low | 6, 10, 19, 20, 71−93 |
| b. We do not recommend using hypotonic solutions like maintenance fluid not even during the resuscitation stage | Strong | Low | 6, 10, 19, 20, 71−93 | |
| Optimization of systemic arterial pressure | a. We suggest the systematic inquiry of he cause of arterial hypotension | Weak | Low | 5, 10, 20, 94−103 |
| b. We suggest using noradrenaline instead of dopamine to keep the target levels of systolic arterial pressure without causing major changes to ICP | Weak | Low | 5, 10, 20, 94−103 | |
| c. In case of arterial hypotension associated with compromised myocardial contractility, we suggest dobutamine as the preferred inotropic agent. | Weak | Low | 5, 10, 20, 94−103 | |
| Management of body temperature | We recommend bringing body temperature down when the level of central temperature >37.5 °C | Strong | Low | 104−115 |
| Maintenance and monitoring of glycemia levels | a. We recommend keeping glycemia levels > 110 and < 180 mg/dL | Strong | Low | 116−134 |
| b. We recommend monitoring the glycemia levels through intensive insulin therapy (80−110 mg/dL) | Strong | Low | 116−134 | |
| Concentration of hemoglobin | We suggest red blood cell transfusion with hemoglobin levels < 7 g/dL except for patients with a compromised cardiac reserve | Weak | Low | 135−159 |
| Maintenance of plasma sodium | We suggest keeping plasma sodium between 135 mEq/L and 145 mEq/L because both hyponatremia and hypernatremia increase the mortality rate | Weak | Low | 160−170 |
| Sedation and analgesia | a. We recommend sedation and analgesia in mechanically ventilated patients | Strong | Moderate | 171−191 |
| b. In patients with TBI on MV who remain hemodynamically stable and with a normal renal function, we suggest analgesia with synthetic opioids (fentanyl, remifentanil) instead of morphine. | Weak | Low | 171−191 | |
| c. During the acute phase, we suggest deep sedation (RASS –4, –5) through the use of propofol or midazolam since both agents improve intracranial variables (ICP, CPP) compared to baseline levels for the lack of convincing tests that one agent is more effective than the other | Weak | Low | 171−191 | |
| d. The use of ketamine is an optional suggestion in normocapnic ventilated patients with hemodynamic instability. | Weak | Low | 171−191 | |
| e. We suggest not running the awakening test in clinically or neurologically unstable patients. | Weak | Low | 171−191 | |
| Prevention of gastrointestinal bleeding | We recommend using proton pump inhibitors in relation to H2-receptor blockers for digestive bleeding prophylaxis. | Strong | Alto | 192−199 |
| Early management of ventilation and oxygenation | a. We recommend orotracheal intubation and mechanical ventilatory support. | Strong | Low | 8, 10, 200−215 |
| b. We recommend normalizing oxygenation and ventilation (SaO2 > 92%, PaO2 > 70 mmHg, pH of 7.35−7.45 and paCO2 of 35−40 mmHg). | Strong | Low | 8, 10, 200−215 | |
| c. We recommend avoiding hypercapnia, hypocapnia and hyperoxia. | Strong | Low | 8, 10, 200−215 | |
| Nutritional aspects | a. We recommend early enteral feeding (24 h–48 h) after the resuscitation stage and after achieving clinical stabilization. | Strong | Low | 216−220 |
| b. We recommend gastric feeding. In case of intolerance or high-risk of aspiration, use prokinetic agents or change into continuous nasojejunal feeding | Strong | Low | 216−220 | |
| c. We suggest enteral feeding regardless of the presence of clinical signs or gastrointestinal contractile activity. | Weak | Low | 216−220 | |
| d. We suggest not using gastric residual volume for tolerance assessments. | Weak | Low | 216−220 | |
| e. We don’t suggest feeding withdrawal in the presence of diarrhea. We suggest looking for the cause. | Weak | Low | 216−220 | |
| f. We suggest to start feeding at a rate of 25−30 kcal/day plus 1.2−2 gr/kg of proteins | Weak | Low | 216−220 |
CPP, cerebral perfusion pressure; MV, mechanical ventilation; MVAP, mechanical ventilation associated pneumonia; PaCO2, partial pressure of carbon dioxide in arterial blood; PaO2, partial pressure of arterial oxygen; pH, hydrogen-ion concentration; ICP, intracranial pressure; RASS, Richmond agitation-sedation scale; SaO2, arterial oxygen saturation.
At the present time, the therapeutic foundations for the management of TBI are grounded on prevention, detection, and early correction of secondary pathological events whether from systemic or intracranial origin that perpetuate or aggravate the primary lesion. Similarly, during the evolution of trauma, different types of complications of various magnitude (tertiary lesions) may arise and eventually worsen the final results in one way or another. For these reasons, developing and maintaining the right physiological environment to promote the recovery of the cerebral parenchyma is one of the primary endpoints. Regardless of the geographical location where the victim of a TBI is assisted and the technology available for specific basic or multimodal monitoring purposes, general care is defined as the common actions that should be implemented in all the centers assisting these victims regardless of the resources available. This document tries to standardize general care for the management of victims of TBI. To our knowledge, this is the first consensus ever achieved on this issue. We should mention though that extensively reviewed topics in former iterations of the clinical practice guidelines published were specifically not included in this version (nutrition, prophylaxis, deep venous thrombosis, etc.).10 Consensus was developed to analyze all the measures implemented to achieve the homeostasis of the body and increase the chances of recovering brain damage, and the actions destined for the general care and prevention of the avoidable complications. The results of a consensus document are useful as long as they are well planned and executed because the suggestions or recommendations that may arise from it will be used in the decision-making process, during the research stage, and when assessing the quality of care. Therefore, the recommendations given in each topic are based on the best evidence available today.
LimitationsConsensus has certain limitations that we should not overlook. Basically, all of them have to do with the methodology used. Actually, there are times that we found a lack of evidence or a low level of evidence available. Also, the methodology used (GRADE) does not exclude the possibility of disagreements or differences of opinion, and there is always a certain degree of subjectivity. In sum, we probably left unanswered questions and unanalyzed topics. Still, we believe our manuscript covers a huge spectrum of general care for the management of TBI.
ConclusionsThis consensus documents with general care measures for the management of TBI included 16 suggestions and another 16 recommendations backed by the strengths or weaknesses of the evidence available in the medical literature and the relevance granted by the working group to every measure, which were mostly backed by a low-quality level.
FundingThis document has received no funding from the industry whatsoever. Instead, it has been economically supported by the personal patrimony of all the authors involved.
Conflicts of interestNone reported.
The authors of this consensus document wish to show their appreciation for the criticism, opinions, and suggestions given by external reviewers who raised the quality of the manuscript.
Therefore, we wish to thank the following professors for their contribution: Alejandro Rabinstein (Rochester, United States), Juan Sahuquillo (Barcelona, Spain); Santiago Lubillo-Montenegro (Tenerife, Spain), Francisco Murillo-Cabezas (Seville, Spain), and José Ignacio Suarez (Baltimore, United States, actual president of the Neurocritical Care Society).
Lastly, I wish to show my personal appreciation and thankfulness for my mentor and friend, professor Francisco Murillo-Cabezas, for helping me during the review phase of our beautiful Spanish language.
Please cite this article as: Godoy DA, Videtta W, Santa Cruz R, Silva X, Aguilera-Rodríguez S, Carreño-Rodríguez JN, et al. Cuidados generales en el manejo del traumatismo craneoencefálico grave: consenso latinoamericano. Med Intensiva. 2020;44:500–508.