The objective was to study the antipyretic and hemodynamic effects of three different drugs used to treat fever in critically ill patients.
MethodsDesign and setting: Prospective, observational study in a 16-bed, general ICU of a university hospital. Patient population: We studied 150 patients who had a febrile episode (temperature >38°C): 50 received paracetamol, 50 metamizol and 50 dexketoprofen. Interventions: None. Body temperature, systolic, diastolic and mean arterial pressure, heart rate, central venous pressure and oxygen saturation were determined at baseline and at 30, 60 and 120minutes after infusion of the drug. Additionally, we recorded temperature 180minutes after starting drug infusion. Diuresis and the need for or change of dose of vasodilator or vasoconstrictor drugs were also recorded.
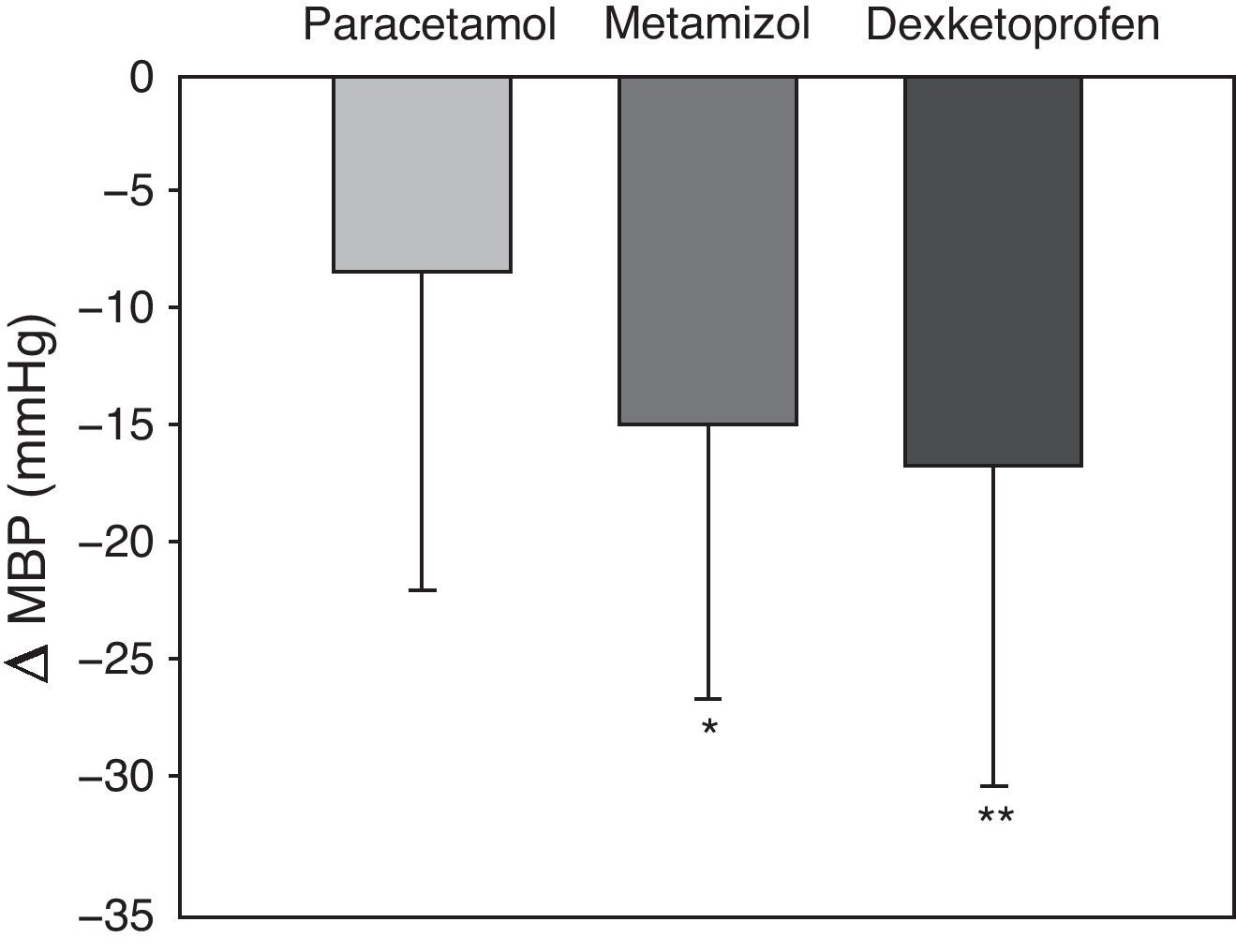
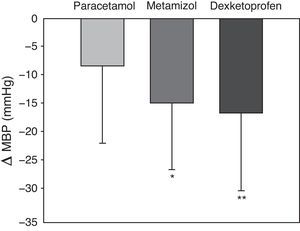
ResultsPatient characteristics, baseline temperature and hemodynamics were similar in all groups. We observed a significant decrease of at least 1°C in temperature after 180minutes in 38 patients treated with dexketoprofen (76%), in 36 with metamizol (72%), and in 20 with paracetamol (40%) (p<0.001). After 120minutes, the mean decrease in mean arterial pressure was 8.5±13.6mmHg with paracetamol, 14.9±11.8mmHg with metamizol, and 16.8±13.7mmHg with dexketoprofen (p=0.005).
ConclusionsDexketoprofen was the most effective antipyretic agent at the doses tested. Although all three drugs reduced mean arterial pressure, the reduction with paracetamol was less pronounced.
El objetivo fue estudiar los efectos antipiréticos y hemodinámicos de 3 fármacos diferentes utilizados para tratar la fiebre en pacientes críticos.
Material y métodoDiseño: estudio prospectivo, observacional, en una UCI de 16 camas de un Hospital Universitario. Pacientes: 150 pacientes que tuvieron un episodio febril (temperatura>38°C). Intervención: 50 recibieron paracetamol, 50 metamizol y 50 dexketoprofeno. Se determinaron la temperatura axilar, presión arterial sistólica, diastólica y media, frecuencia cardíaca, presión venosa central y saturación de oxígeno, en situación basal y a los 30, 60 y 120 minutos tras la administración del fármaco. También se registró la temperatura a los 180 minutos después de haber iniciado el fármaco. La diuresis y las necesidades de tratamiento vasodilatador y vasoconstrictor durante el tratamiento también se registraron.
ResultadosLas características de los pacientes, la temperatura y la hemodinámica basal fueron similares en todos los grupos. Observamos un descenso significativo de al menos un grado en la temperatura después de 180 minutos en 38 pacientes tratados con dexketoprofeno (76%), en 36 con metamizol (72%), y en 20 con paracetamol (40%) (p<0,001). Después de 120 minutos, la media del descenso de la presión arterial media fue de 8,5±13,6mmHg con paracetamol, 14,9±11,8mmHg con metamizol y 16,8±13,7mmHg con dexketoprofeno (p=0,005).
ConclusionesDexketoprofeno fue el fármaco antipirético más efectivo, a las dosis estudiadas. Aunque los 3 fármacos redujeron la tensión arterial media, la reducción con paracetamol fue menos pronunciada.
Fever is common in critical patients, and is observed in 90% of all septic patients.1,2 A febrile episode may be of infectious or non-infectious origin. Pneumonia, sinusitis and bacteremia (primary or catheter-related) are the most frequent infectious causes of fever, while the non-infectious origins include cancer, drugs, transfusions and allergic reactions.3
The initial management of fever includes treatment of the cause and the administration of antipyretic (fever-lowering) drugs. Antipyretic treatments are effective in lowering temperature, but can have important side effects.4 Such drugs should not be used on a routine basis in the Intensive Care Unit (ICU). The risks and benefits should be evaluated individually in each fever episode. Paracetamol is simple to administer and is safe, with a high therapeutic index and a low risk of side effects in the form of renal, gastrointestinal or hematological disorders.5 Metamizol in turn is usually used to treat postoperative pain and fever. Dexketoprofen is a water-soluble salt of ketoprofen, a dextrorotary enantiomer belonging to the group of nonsteroidal antiinflammatory drugs (NSAIDs). It is used as an analgesic and antiinflammatory agent, and in vitro constitutes one of the most potent inhibitors of prostaglandin synthesis.6 To date, the antipyretic effect of dexketoprofen has only been described in animal models.7 This drug substance has been compared with other NSAIDs in the management of postoperative pain. It appears to be better tolerated than other NSAIDs,8 but its antipyretic effect and hemodynamic profile in critical patients have not been described.
The present study compares the antipyretic and hemodynamic effects of paracetamol, metamizol and dexketoprofen–the main drugs used to treat fever in critical patients.
Patients and methodsA prospective observational study was carried out in the 16-bed ICU of a University hospital between 2005 and April 2007, involving 150 patients with an episode of fever (over 38°C) which the supervising physician decided to treat using one of the three drugs employed in the Unit for this purpose. Each patient was included in the study only once. The decision to treat was established in each patient based on the clinical repercussions of fever: tachypnea, tachycardia, changes in blood pressure and increased production of carbon dioxide or oxygen consumption. The antipyretic treatments commonly used in our Unit for fever are paracetamol 1000mg, metamizol 2000mg and dexketoprofen 50mg – all administered as an intravenous infusion during 30minutes. An ethics committee of our hospital approved the study without the need for informed consent. The following variables were monitored at baseline (immediately prior to the start of treatment) and 30, 60 and 120minutes after infusion of the drug: axillary temperature, systolic blood pressure, diastolic blood pressure, mean blood pressure (MBP), heart rate (HR) and oxygen saturation (SatO2) measured by pulsioximetry. Temperature was monitored 180minutes after infusion of the drug to determine a decrease of at least 1°C. Blood pressure was recorded using an invasive system in those patients in which such a system was already in place, based on a femoral or radial arterial catheter, and noninvasively using a digital arm sphygmomanometer in the rest of the cases. The pressure measurement system of a given patient was not modified in the course of the different measurements. Diuresis was recorded from baseline and up to 120minutes. We also documented the requirements referred to vasopressor drugs, vasodilators and fluid therapy before treatment and during 120minutes after infusion. Likewise, the SAPS (Simplified Acute Physiology Score) II9 was recorded upon admission, along with the reason for admission and the need for mechanical ventilation (MV) at the time of the study.
The sample size calculated to detect a decrease of 1°C in temperature was 50 patients per group, with a type I error of 5% (α=0.05) and a statistical power of 80% (β=0.20). The patients were included in the study until completion of the assigned 50 subjects per group. The quantitative variables were subjected to analysis of variance (ANOVA), while the chi-squared test was used to analyze the qualitative variables. A two-factors ANOVA was used with the general linear model (GLM). The factors were: time (start of the study, 30, 60 and 120minutes), treatment (paracetamol, metamizol and dexketoprofen) and their interaction, which would serve to answer the question of whether the evolution of the treatments differed in the course of follow-up. A post hoc analysis was performed where necessary. In addition, ANOVA was used to compare the decrease in MBP with each treatment from baseline and up to 120minutes. Statistical significance was considered for p<0.05. The SPSS version 14.0.1 statistical package (SPSS Inc., Chicago, IL, USA) was used throughout.
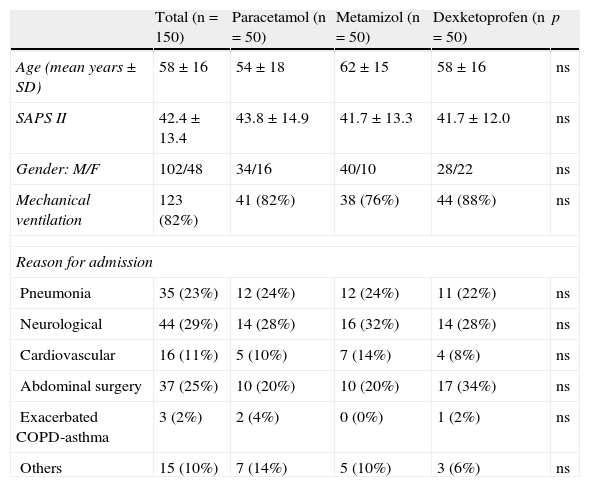
ResultsOf the 150 patients studied, 102 were males (68%) and 48 females (32%). The mean age was 58±16 years (range 19–86). The SAPS II score was 42.4±13.4. Each group (paracetamol, metamizol and dexketoprofen) comprised 50 patients. The demographic characteristics are shown in Table 1. There were no statistically significant differences between the groups for any of these variables. All enrolled patients completed the study.
Patient characteristics at baseline and per treatment group. There were no statistically significant differences between the groups.
| Total (n=150) | Paracetamol (n=50) | Metamizol (n=50) | Dexketoprofen (n=50) | p | |
| Age (mean years±SD) | 58±16 | 54±18 | 62±15 | 58±16 | ns |
| SAPS II | 42.4±13.4 | 43.8±14.9 | 41.7±13.3 | 41.7±12.0 | ns |
| Gender: M/F | 102/48 | 34/16 | 40/10 | 28/22 | ns |
| Mechanical ventilation | 123 (82%) | 41 (82%) | 38 (76%) | 44 (88%) | ns |
| Reason for admission | |||||
| Pneumonia | 35 (23%) | 12 (24%) | 12 (24%) | 11 (22%) | ns |
| Neurological | 44 (29%) | 14 (28%) | 16 (32%) | 14 (28%) | ns |
| Cardiovascular | 16 (11%) | 5 (10%) | 7 (14%) | 4 (8%) | ns |
| Abdominal surgery | 37 (25%) | 10 (20%) | 10 (20%) | 17 (34%) | ns |
| Exacerbated COPD-asthma | 3 (2%) | 2 (4%) | 0 (0%) | 1 (2%) | ns |
| Others | 15 (10%) | 7 (14%) | 5 (10%) | 3 (6%) | ns |
SD: standard deviation; COPD: chronic obstructive pulmonary disease; M: male; F: female; ns: nonsignificant; SAPS: Simplified Acute Physiology Score.
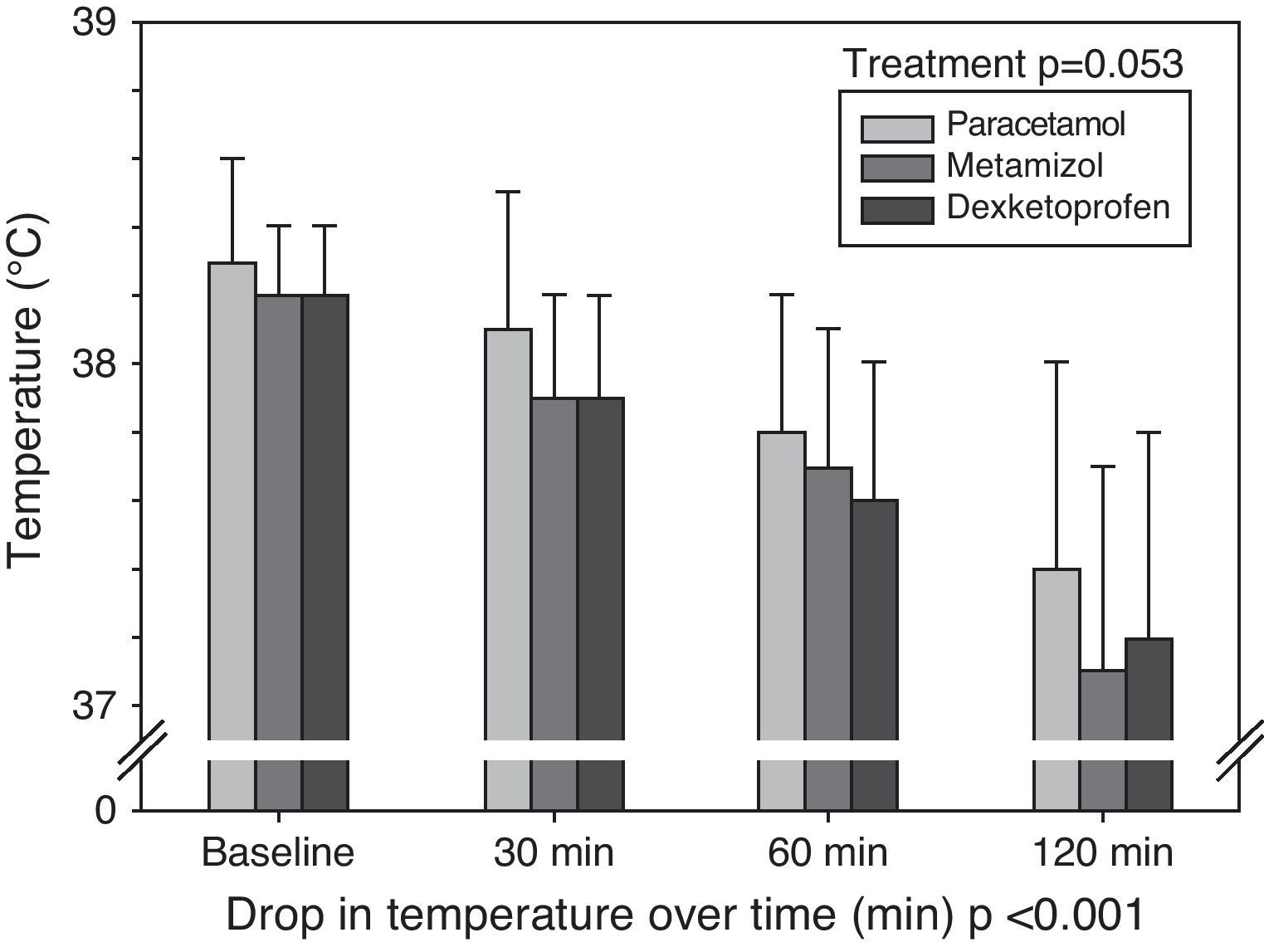
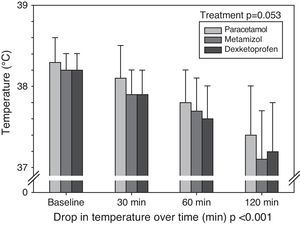
We recorded a significant decrease in temperature of at least 1°C after 180minutes in 38 patients treated with dexketoprofen (76%), in 36 treated with metamizol (72%) and in 20 treated with paracetamol (40%) (p<0.001). In 37% of the patients no decrease of at least 1°C was observed after 180minutes. Fig. 1 shows the mean decrease in temperature in each group at the four timepoints, while Table 2 documents the mean and standard deviation of the temperature drop for each drug and at each of the studied timepoints. A significant decrease in temperature was recorded over time, but there were no interactions among the three different therapies over time – i.e., none of the treatments lowered body temperature more than the rest at any of the timepoints.
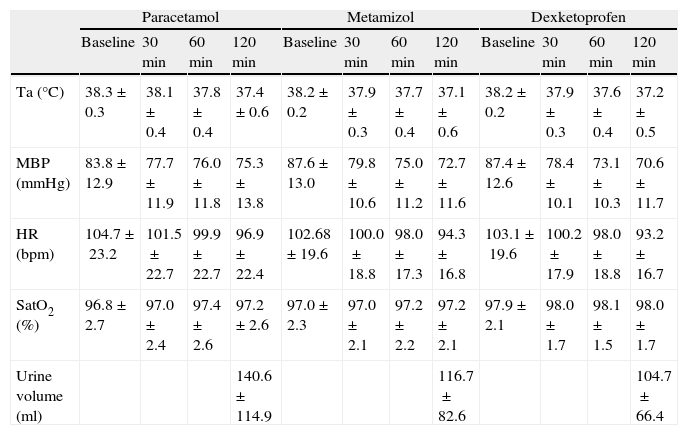
Axillary temperature, mean blood pressure, heart rate, oxygen saturation determined by pulsioxymetry at baseline and after 30, 60 and 120minutes, and diuresis from baseline to 120minutes.
| Paracetamol | Metamizol | Dexketoprofen | ||||||||||
| Baseline | 30min | 60min | 120min | Baseline | 30min | 60min | 120min | Baseline | 30min | 60min | 120min | |
| Ta (°C) | 38.3±0.3 | 38.1±0.4 | 37.8±0.4 | 37.4±0.6 | 38.2±0.2 | 37.9±0.3 | 37.7±0.4 | 37.1±0.6 | 38.2±0.2 | 37.9±0.3 | 37.6±0.4 | 37.2±0.5 |
| MBP (mmHg) | 83.8±12.9 | 77.7±11.9 | 76.0±11.8 | 75.3±13.8 | 87.6±13.0 | 79.8±10.6 | 75.0±11.2 | 72.7±11.6 | 87.4±12.6 | 78.4±10.1 | 73.1±10.3 | 70.6±11.7 |
| HR (bpm) | 104.7±23.2 | 101.5±22.7 | 99.9±22.7 | 96.9±22.4 | 102.68±19.6 | 100.0±18.8 | 98.0±17.3 | 94.3±16.8 | 103.1±19.6 | 100.2±17.9 | 98.0±18.8 | 93.2±16.7 |
| SatO2 (%) | 96.8±2.7 | 97.0±2.4 | 97.4±2.6 | 97.2±2.6 | 97.0±2.3 | 97.0±2.1 | 97.2±2.2 | 97.2±2.1 | 97.9±2.1 | 98.0±1.7 | 98.1±1.5 | 98.0±1.7 |
| Urine volume (ml) | 140.6±114.9 | 116.7±82.6 | 104.7±66.4 | |||||||||
All values expressed as the mean±standard deviation. p=nonsignificant for all variable studied.
HR: heart rate; bpm: beats per minute; min: minutes; MBP: mean blood pressure; SatO2: oxygen saturation; Ta: axillary temperature.
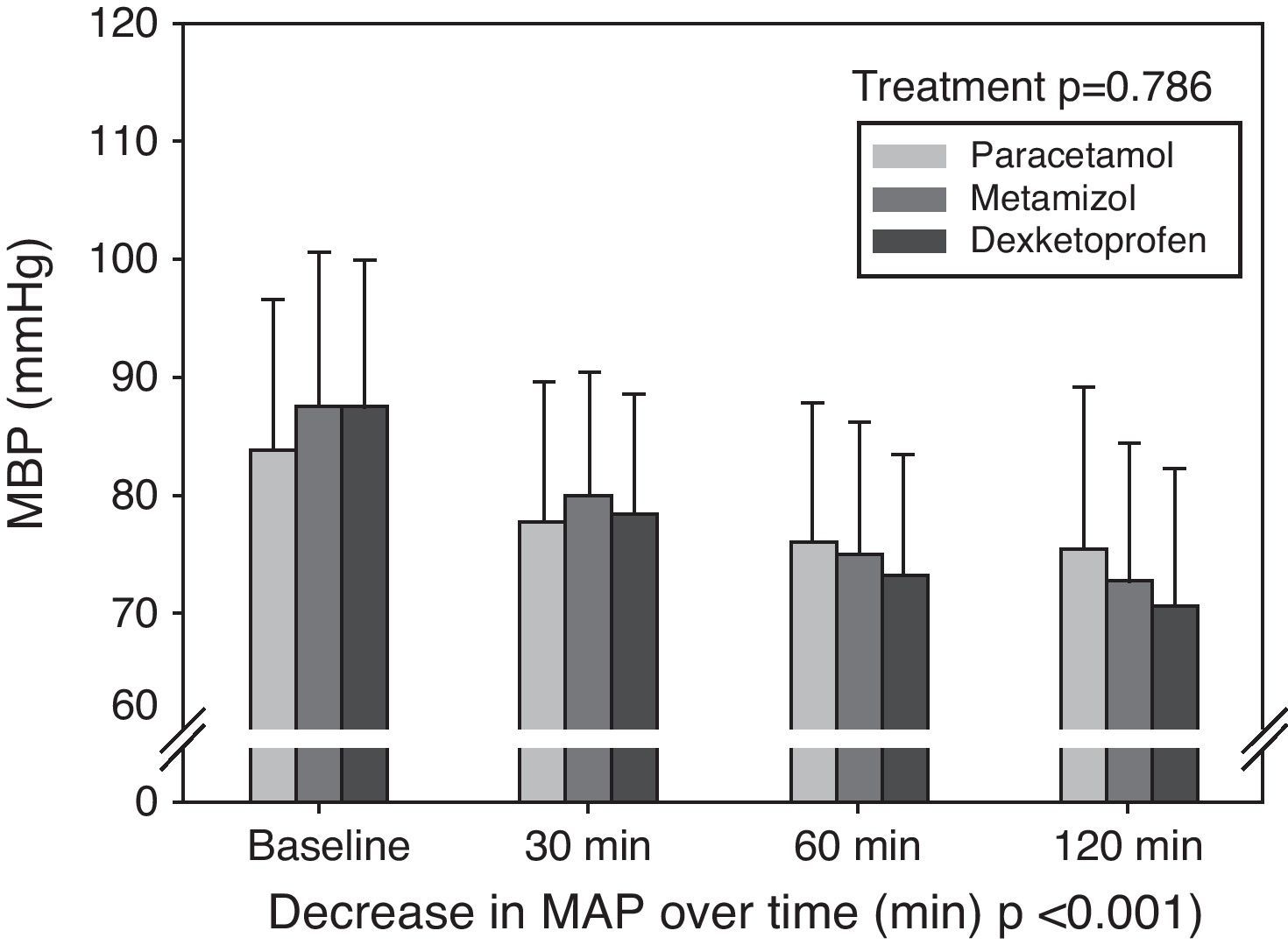
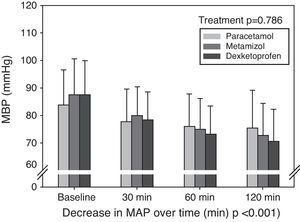
The systemic hemodynamic variables are shown in Table 2, expressed as the mean and standard deviation. There were no statistically significant differences between the groups in terms of mean blood pressure, oxygen saturation determined by pulsioxymetry or heart rate at the different timepoints studied and for each antipyretic drug. Likewise, there were no differences in diuresis recorded during the study period among the different treatments. Fig. 2 shows the evolution of MBP±standard deviation at the four timepoints (baseline, and after 30, 60 and 120minutes) in each of the three groups. There were no statistically significant differences between the treatments at any timepoint. A significant decrease in MBP was recorded over time, with interaction of the three different treatments in time. Fig. 3 shows the mean decrease in MBP in each group. After 120minutes, the mean decrease in MBP was 8.5±13.6mmHg with paracetamol, 14.9±11.8mmHg with metamizol, and 16.8±13.7mmHg with dexketoprofen (p=0.005). The post hoc analysis showed the drop in MBP in the paracetamol group to be smaller than in the metamizol and dexketoprofen groups, while no statistically significant differences were recorded between the metamizol and dexketoprofen groups.
Thirty-nine of the 150 patients (26%) were receiving vasoconstrictors during the fever episode: 15 in the paracetamol group (38.5%), 9 in the metamizol group (23%) and 15 in the dexketoprofen group (38.5%). Of these 39 patients, one in the paracetamol group was receiving adrenalin, one in the metamizol group was receiving dopamine, and the rest were all receiving noradrenalin at the doses required to keep the mean blood pressure above 65mmHg. After starting antipyretic treatment, 10 of 15 patients treated with paracetamol (66%), including the patient receiving adrenalin, required an increase in vasoconstrictor dose. Seven of the 9 patients in the metamizol group (77%) and 12 of the 15 patients in the dexketoprofen group (80%) required an increase in noradrenalin dose. Vasopressor treatment was started to maintain adequate systemic blood pressure in 7 patients: one in the paracetamol group, two in the metamizol group and four in the dexketoprofen group. Twenty-eight of the 150 patients (18.7%) were receiving vasodilators in continuous infusion with nitroprussiate or labetalol: 10 in the paracetamol group (35.7%), 11 in the metamizol group (39.3%) and 7 in the dexketoprofen group (25%). The vasodilator dosage had to be lowered in 6 of the 10 patients treated with paracetamol (60%), in 9 of the 11 patients treated with metamizol (81.8%), and in 5 of the 7 patients treated with dexketoprofen (71.4%). In 7 of the patients receiving vasodilators, the treatment had to be suspended: three in the paracetamol group, three in the metamizol group and one in the dexketoprofen group. None of these patients required the start of vasoconstrictor treatment. There were no statistically significant differences in the need for vasoconstrictor increments or for a lowering of vasodilator dose between the groups, and in all patients the aim was to maintain the mean blood pressure above 65mmHg.
Fifteen of the 150 patients (10%) required fluid therapy while receiving antipyretic treatment, in order to avoid an excessive drop in blood pressure. Four patients in the paracetamol group, 5 in the metamizol group and 6 in the dexketoprofen group required the administration of 250–500ml of crystalloids, administered during 30minutes after detecting the decrease in blood pressure.
Twenty patients suffered acute renal failure and required hemodialysis before antipyretic treatment: 8 in the paracetamol group, 5 in the metamizol group and 7 in the dexketoprofen group. After antipyretic treatment, a total of 5 additional patients required hemodialysis: four in the paracetamol group and one in the dexketoprofen group. None of the patients were connected to the dialysis system during the study.
DiscussionThe main findings of this observational study were that paracetamol appeared to be the best of the three studied drugs in terms of a lesser reduction in MBP. However, paracetamol only proved capable of lowering temperature by at least 1°C after 180minutes in less than one-half of the patients. These findings suggest that it may be the drug of choice in the treatment of a fever episode when the patient is hemodynamically unstable, although a significant decrease in temperature is unlikely. In patients under hemodynamically stable conditions, metamizol or dexketoprofen could be the first choice for lowering temperature, due to the greater percentage success with these drugs compared with paracetamol. In those patients in which temperature did not decrease (37%), we do not know what the course would have been without the administration of antipyretic treatment.
Although physical cooling measures are effective in reducing skin temperature when the physiological thermoregulation mechanisms are altered, such measures do not lower the thermoregulatory center temperature setting, and moreover can increase discomfort and metabolic stress in non-sedated febrile patients.10
Our study was carried out with three commonly used drug substances: paracetamol, metamizol and dexketoprofen. A number of studies in the literature have compared changes in temperature and the hemodynamic effects of drugs used for the treatment of fever. The antipyretic effects of metamizol and paracetamol have been described elsewhere.11–15 Poblete et al.14 found that paracetamol and metamizol do not induce clinically significant temperature reductions in critical patients with fever, compared with the adoption of physical cooling measures. However, Gozzoli et al.16 compared these same drugs, i.e., metamizol and paracetamol, with physical measures in the treatment of fever, and found all three treatments to lower temperature equally. As in our study, these authors concluded that metamizol should not be regarded as the first choice antipyretic drug in hemodynamically unstable patients, and that paracetamol should be preferred in such cases. The discrepancies between the studies of Poblete and Gozzoli are probably due to the small number of patients studied in each group: 20 in the first and 30 in the second. Oborilová et al.11 in turn studied 254 fever episodes, fundamentally in hemato-oncological patients treated with metamizol, diclofenac and paracetamol. They found all these drugs to offer a significant antipyretic effect, though metamizol proved better than paracetamol in improving patient discomfort associated to fever. However, this study did not include critical patients and, on the other hand, since these were hemato-oncological patients, the immune alterations produced by the tumor disease or by the associated treatment could have influenced the temperature values.
In our study all three drug substances lowered MBP. Of 39 patients receiving vasoconstrictor treatment, a large percentage in each group required a drug dose increment, and vasoconstrictor treatment had to be started in 7 patients. Of the total of 28 patients receiving vasodilators, the drug dose had to be lowered in a large proportion of patients and suspended in 7 of the 28 subjects. In this group of patients, the hypotensive effect of the antipyretic drugs may have been magnified by the concomitant infusion of a vasodilator drug. However, since a low percentage of patients was involved, with a homogeneous distribution among all treatment groups, we suspect that this effect is scantly relevant in terms of the end result. Despite these hemodynamic changes, diuresis was not modified during the 120minutes of follow-up. These results are comparable to those of others in which metamizol induced a significant decrease in MBP compared with paracetamol. Using metamizol, ketorolac and paracetamol as treatment for postoperative pain in critical patients, Avellaneda et al.17 reported a decrease in radial blood pressure in all three treatment groups, while Hoigné et al.18 registered a significant drop in systolic pressure in patients treated with metamizol.
Cruz et al.15 also described a decrease in MBP and in other hemodynamic variables after the administration of metamizol or paracetamol in 60 patients with fever. In the case of hypotension induced by metamizol, this was explained by the relaxing effect of the drug upon the smooth muscle cells, resulting in peripheral vasodilatation.16
Our study has a number of limitations. A first consideration is the study design involved. Since this is an observational and not a randomized or masked study, the results obtained are not conclusive. The choice of antipyretic treatment based on the decision of the supervising physician may have introduced drug–patient selection bias. On the other hand, since the effects of the three drug substances were not compared with the adoption of physical cooling measures as in other studies, the comparison possibilities are limited. In turn, we recorded axillary temperature but not core temperature–the latter only being routinely registered in our ICU once or twice a day. On the other hand, the American College of Critical Care Medicine and the Infectious Diseases Society of America define fever as a temperature of over 38.3°C.19 In our ICU, however, we treat patients with temperatures of 38°C or higher and with clinical repercussions. Our study only reflects our daily clinical practice. In turn, the administered drug dose was not calculated according to body weight, and the prescribed standard dose may have influenced the results. Likewise, no registries were made of pain. In our ICU, patients subjected to mechanical ventilation receive sedation and analgesia in order to maintain a Ramsay Sedation Scale20 score of between 2 and 3. In our series, 123 patients were on mechanical ventilation at the time of the fever episode, but we do not have specific data referred to the situation of pain among the included patients; a hemodynamic effect of pain therefore cannot be discarded.
It is not clear whether fever in itself is beneficial or harmful.4,21 Studies in animals with infection describe fever as being beneficial, and there is no evidence that the administration of antipyretic drugs modifies mortality.1 Fever complements the host immune defenses against infection22 and activates some immune function parameters, with the activation of T cells, cytokine production and antibodies, and neutrophil and macrophage function.23 On the other hand, an elevated body temperature may be associated to a range of deleterious effects such as increased cardiac output, oxygen consumption and carbon dioxide production. These changes may be poorly tolerated by critical patients with a limited cardiorespiratory reserve.24 The negative hemodynamic and metabolic effects of fever are particularly undesirable in the presence of heart problems or in situations of clinical sepsis, in which myocardial function is depressed.25 Moreover, during or after a period of brain ischemia or trauma, hyperthermia markedly increases the resulting neuronal damage.26 All these data suggest that the treatment of a fever episode should be evaluated individually taking into account the benefits and possible side effects.27
In sum, dexketoprofen and metamizol exhibited a better antipyretic effect at the studied doses, but with a poorer hemodynamic profile. In contrast, paracetamol was associated with increased hemodynamic stability but with a lesser antipyretic effect. The characteristics of each individual patient should be taken into account when prescribing an antipyretic drug, in order to avoid hemodynamic instability. Nevertheless, further studies are needed, involving a randomized design, in order to be able to draw firm conclusions.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vera P, et al. Efectos hemodinámicos y antipiréticos del paracetamol, metamizol y dexketoprofeno en pacientes críticos. Med Intensiva. 2012;36:619–25.