Suffering is not only exclusive to patients or their relatives, but also to the health professionals, who feel to be at the center of the depersonalization process. Over-technification and the fact that the disease process is sometimes the only focal point of our activities, together with the ever-increasing influence of institutional power seen in recent times, all cause the health professional to be the first in demanding a change in health institution dynamics. Following initial reflection from one of the most technified medical specialties (Intensive Care Medicine), classically isolated from the rest of the Hospital and from the community, we implemented a project aimed at securing integration and empathy in our approach to patients and their relatives in the Intensive Care Unit (ICU) of Infanta Margarita Hospital. The project was designed to incorporate tools for working on the most important elements of a humanization plan, i.e., the patients, their relatives, the health professionals and the community, attempting to disclose the work done in the ICU over a period of 12 months. This project is referred to as the Project ICU Infanta Margarita: 1 year: 12 months for 12 commitments.
La humanización en sanidad surge por la necesidad de acercarnos a una dimensión más holística de la enfermedad. El sufrimiento no solo es exclusivo de los pacientes y las familias, sino que el profesional se encuentra en el centro del proceso de despersonalización. El exceso de tecnificación y la colocación del proceso patológico en ocasiones como único objetivo de actuación, así como la hipertrofia del poder institucional que estamos viviendo en los últimos tiempos, hacen que en ocasiones el propio profesional sanitario sea el primero en demandar un cambio en el abordaje de la dinámica dentro de las instituciones sanitarias. Tras una reflexión inicial, desde el corazón de la medicina más tecnificada, como es la Medicina Intensiva, clásicamente aislada del resto del entorno hospitalario y de las familias, decidimos abordar un proyecto de integración, empatía y acercamiento a los pacientes y familiares de la Unidad de Cuidados Intensivos (UCI) del Hospital Infanta Margarita, en el que se pretendieron implementar herramientas para trabajar en los elementos más importantes de un plan de humanización (las familias, pacientes, profesionales, y nuestra comunidad), potenciando el dar a conocer el trabajo que se realiza en la UCI y que se desarrolló a lo largo de 12 meses, el proyecto: UCI Infanta Margarita, 1 año: 12 meses para 12 compromisos.
The need for humanization is currently patent in many settings in both private and professional life–not only in the field of healthcare but also in many other professions. Nevertheless, healthcare is possibly the scenario where the situation proves most delicate, since vulnerability and suffering are almost inherent to the disease process. The healthcare changes of recent years have generated much debate regarding humanization in the care of ill people.1 The term “humanize” is sometimes controversial, despite the fact that it is an intrinsic part of the healthcare profession.2 In strict terms, the Royal Spanish Academy (Academia Real Española [RAE]) defines the term as: to make something or someone human, familiar and affable. On the other hand, it can also be taken to mean to soften, free from anger, or become benign.
Humanization in healthcare is not an ideology: it is an alliance with the person and his or her way of living. It entails aspects referred to quality and constitutes an ethical commitment to consider an individual in its entirety: both in relation to autonomy and in its more subjective dimension. In order to humanize in healthcare we must respect the fact that each person is unique and unrepeatable, and responds differently to life crises.3 A range of settings therefore must be addressed: healthcare (care and caregiver), ethical, cultural, professional competence (communication, skills), as well as human resources.
Humanizing is related to the environment (spaces, wellbeing, warmth), competence and collaboration interventions, integration in the community, the individual and collectivity. All this implies the need to include human sciences in the training of healthcare staff and, of course, to protect the right to retain control of one's own life.
In contrast, dehumanization means depersonalization, and views the disease process as the sole target of medical care. Some of the main causes of dehumanization are: the “dictatorship of technology”, which leads to patients being seen as “things”; super-specialization; the application of economical value-based criteria to healthcare management; and the negation that suffering and death affect patients, relatives and professionals equally.3
The intensive use of technology may have caused the humans needs of patients, relatives and professionals to be seen as a secondary concern.2,4 For this reason, from the core of the most technified medical practice, from the sophistication and strict organization of Intensive Care, we postulate the need to compatibilize and accompany the incorporation of technological and scientific advances with the best of human values.
In this context, and following initial reflection, we decided to implement a humanization project in the Intensive Care unit (ICU) of Infanta Margarita Hospital (Córdoba, Spain), called Project ICU Infanta Margarita Hospital: 1 year: 12 months for 12 commitments.
This ambitious project was designed to implicate all the professionals in the ICU–physicians, nurses and assistant staff, with their exceptional commitment qualities.
It constitutes a solidary initiative for integration and closeness with the patients and their families, seeking to become aligned with them, their needs and expectations, opening our Unit and making purely professional care compatible with much more personalized attention.
In addition to improving in our profession, we established other objectives:
- 1.
To make the specialty of Intensive Care Medicine and the work in the ICU known.
- 2.
To improve communication, not only among the professionals of the Unit but also with the rest of the professionals in the hospital setting and in our healthcare area, and with our patients and their relatives.
- 3.
To promote motivation at work, seeking tools to care for the professionals.
In sum, the aim was to secure a greater presence in the community.
Conception and development of the projectThe ICU of Infanta Margarita Hospital comprises of 12 rooms, and registers approximately 400 admissions a year (polyvalent disease and coronary patients) in the setting of a 230-bed district hospital with a recruitment population of 150,000 inhabitants. The Unit was created in 2010, with a modern structure, and with relatively young and highly motivated physicians and nursing staff.
At the start of the project we established a number of prior premises:
- -
The presence of a sensitized team, with previous initiatives seeking to ensure a more open ICU.
- -
Experience with works done and presented at congresses in topics such as patient intimacy or the prevention of posttraumatic stress disorder.
- -
A strongly favorable physical structure. A humanized infrastructure affords optimum environmental and physical wellbeing for patients, professionals and families, with spaces that are functional, efficient, ergonomic, comfortable, warm and friendly.5 This is a Unit with individual boxes, large windows and natural light, ample spaces for the work of the professionals and the families, as well as information offices offering intimacy and privacy.
The following actions were taken to implement the project:
- 1.
A group of professionals with special concerns in humanization topics was identified through informal team conversations.
- 2.
Work meetings with the members of the Unit were organized.
- 3.
A leader was designated, with special sensitivity, communication skills, empathy with the team, and interest in the project, being in charge of distributing tasks and supervising all the working groups.
- 4.
The contributions of the group and the initiatives of the leader served to develop a working plan and calendar.
- 5.
The project was designed in late 2015, with the definition of a series of monthly commitments. A voluntary collaboration list was established. Each commitment was assigned to at least two individuals in charge and from different sectors, depending on the topic in question.
- 6.
The intermediate supervisors (Unit management-supervision) were placed in charge of the administrative issues, communication with Hospital Management, external contacts (town halls, communications media, etc.) and global coordination.
- 7.
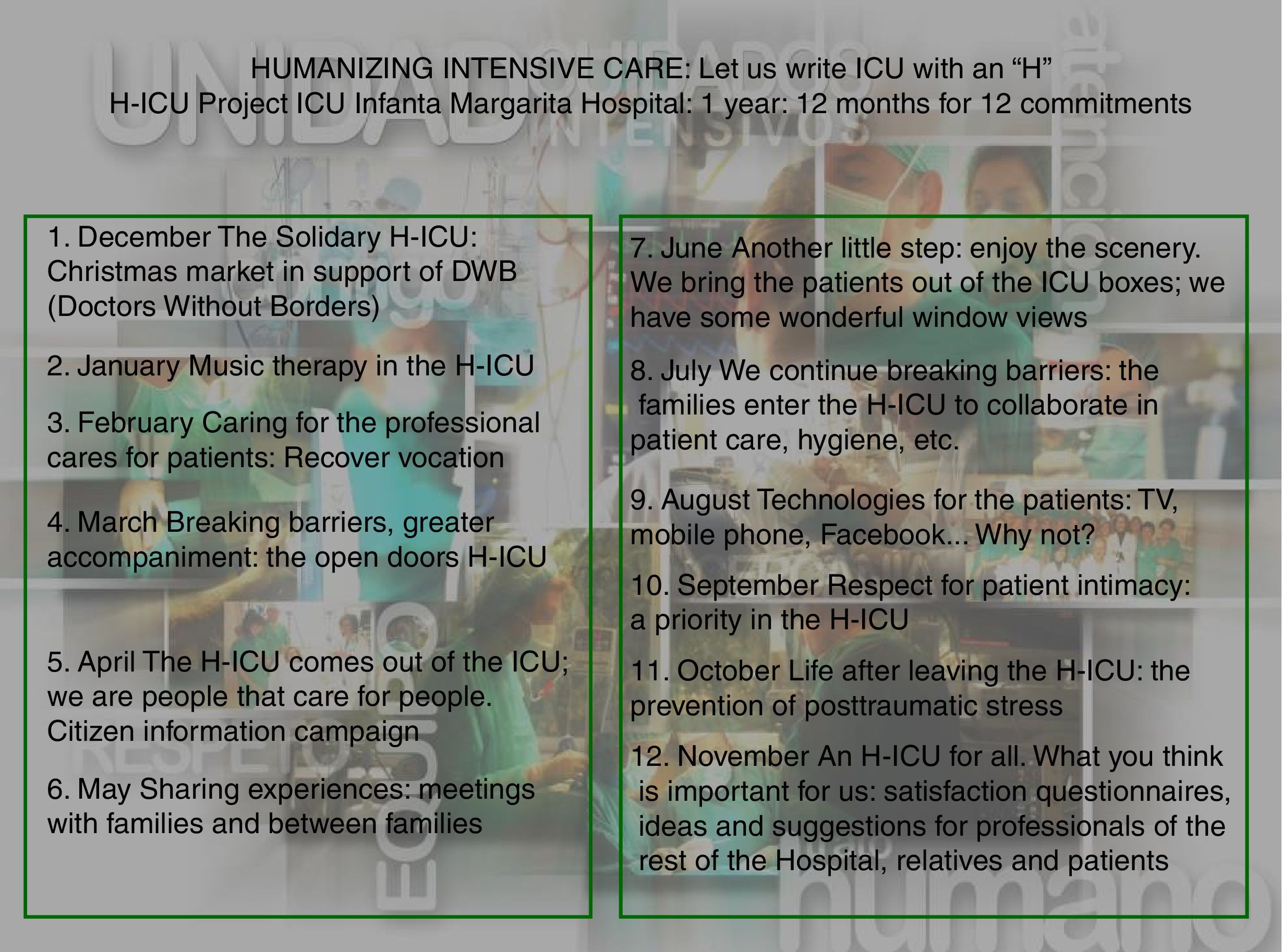
The project was presented to Hospital Management. Following approval, we started both external and internal diffusion of the initiative, largely using resources of our own: posters (Fig. 1), press releases, a monthly local and regional radio program, and television reports.
- 8.
Due to the importance of the social networks, the key point for making the project known was the creation of a page in Facebook,6 managed by the project leader, with the aim of reaching as many professionals and healthcare users as possible, and of making us known to other humanization projects and initiatives in different healthcare settings. On a monthly basis, the page displayed our activities, projects and images of the plan, as well as the contributions of patients, relatives and healthcare staff, with the consolidation of over one thousand followers.
- 9.
We opened the doors of the UCI to colleagues from other hospitals wishing to learn about the project, and we shared our experiences in working sessions. We decided to start in December, coinciding with the Christmas holidays, and the project was thus scheduled to end in November 2016.
Implementation of the project is described below, along with some of the evidences referred to our work.
Implementation of the project1. December: The Solidary H-ICU: Christmas market in support of DWB (Doctors Without Borders)BackgroundIn previous years and coinciding with the Christmas holidays, the UCI organized a special humanitarian event in the setting of Intensive Care.
We felt that the best way to start our project was to talk about solidarity. We wished to make it known through this “first commitment”, and considered the best destination to be Doctors Without Borders (DWB) – colleagues who one day decided to take a step further and pursue their vocation to its ultimate consequences. We could look to them to further strengthen vocation, because we can all be DWB, even without having to leave our own setting – giving the best of ourselves to those around us who are suffering: The Solidary H-ICU.
InterventionThis year as solidary commitment we decided to organize a little market, during several days, both in the vicinity of the Hospital and in the center of the city. The work and donations of the objects sold were exclusively contributed by the professionals in the Unit, and the money obtained was exclusively dedicated to DWB.
ResultsWe have received many thanks and words of appreciation from DWB, with diffusion through their networks.
From the start of the project we have continued to collaborate with them, disclosing their activities – fundamentally through our page in Facebook – and participating in other financial collaborations and initiatives that are regularly repeated in Christmas.
2. January: Music therapy in the H-ICUBackgroundMany studies have shown the excessive use of opioid analgesics and sedatives to be associated to adverse effects–some of which can prove serious. Such drugs prolong mechanical ventilation and ICU stay, and increase the nosocomial pneumonia and mortality rates.7 Non-pharmacological measures, such as music therapy, can help not only to reduce the doses of medication but also to make our Unit a less hostile environment, establishing new routes of communication with our patients and facilitating forms of expression. The capacity of music to lessen stress and anxiety is well known, both in conscious patients and individuals that are sedated and subjected to mechanical ventilation–resulting in improvement of the physiological parameters such as respiratory frequency, heart rate and both systolic and diastolic blood pressure.8 Pain and anxiety have been evaluated using different scales, such as the visual analog scale (VAS) or the Spielberger State-Trait Anxiety Inventory (STAI), and many studies have moreover shown music therapy to offer clear benefits.9,10 In this regard, a series of biological benefits have been described, such as a decrease in cortisol or prolactin levels, allowing the reduction of sedatives in mechanically ventilated patients enrolled in a music therapy intervention.11
The World Federation of Music Therapy defines music therapy as: “The use of music and/or musical elements (sound, rhythm, melody, harmony) by a qualified music therapist in a patient or group, in the context of a process designed to facilitate and promote communication, relationships, learning, mobilization, expression, organization and other relevant therapeutic objectives, with a view to achieving changes and satisfying physical, emotional, mental, social and cognitive needs”.
Music therapy in our Unit is conceived as a complementary measure of help in controlling stressing factors in our patients.12 The main objective therefore was to lessen stress and pain, regulate the hours of sleep, and avoid delirium as well as fear of transfers, invasive treatments, or the facing of death.
InterventionWe started this commitment in January with a series of “Music therapy in the ICU” sessions, joining the views of different professionals such as intensivists, nurses, music therapists and professional musicians.
Following this initiative, we created a working group (comprising a nurse, an intensivist and a music therapist) with the purpose of defining a protocol, an intervention form and data collection sheet.
Given the voluntary nature of the work of the music therapy professional, a weekly visit is scheduled, occupying a full morning, in which patients that are hoped to benefit from the intervention (subjects with high-dose sedatives, weaning problems, agitation and delirium) are selected by the intensivists and nursing staff.
In an individualized session, the specialist (Fig. 1 of Annex 1. Supplementary material) works with the patient and/or family, compiling a “musical biographic history” to be used in defining therapeutic objectives between the care team and the music therapist. Another part of the session explores the physiological reactions of the patient using music therapy tools (certain music instruments), creating a new route of communication. All this is reflected on a data collection sheet that records the physiological responses (heart rate, respiratory frequency, blood pressure, etc.) and which is entered in the patient clinical history, with the prescription of a series of instructions according to nursing shifts (e.g., type of music indicated for relaxation, the induction of sleep, etc.). The complete therapy session, including the family interview, usually lasts a little over one hour.
In most cases, the families are an important part of the process and feel that they are participating in the care of the patient.
In this regard, the nurse in the working group was specifically trained in “Music therapy as a nursing intervention”, and workshops were held to offer training in exploring the emotional wellbeing of patients in the ICU (sleep, delirium, pain, anxiety) and the use of music as a care measure.
ResultsMusic already forms part of the care of the patients in the ICU, and has received great acceptance on the part of both the patients and families. The interventions of the therapist have afforded great benefits and are pending an in-depth analysis.
3. February: Caring for the professional cares for patients: recover vocationBackgroundWorking in an ICU can be particularly stressing. According to some studies, “burnout syndrome” can affect up to 50% of the professionals that work in such Units. The classical symptoms are tiredness, depersonalization and loss of self-esteem. A number of risk factors have been identified, such as an excessive work burden, scant recognition, continuous contact with life-threatening situations, and end-of-life events. All this in turn can give rise to tiredness, anxiety and depression.13
We view the care of the professional as a necessary measure in order to guarantee the quality of patient care, seeking motivation and the recovery of vocation in many cases.
Another objective was to gain awareness of the communication problems with the families and among professionals, and to afford training in communication tools. Many studies have evidenced shortcomings in this respect. There is a lack of comprehension in diagnosis, prognosis and treatment in nearly 40% of all cases.14,15 Training and the acquisition of communication skills should be mandatory in the preparation of healthcare professionals. Interventions in this area, such as the training of medical students, have led to improvements.16 We not only need to improve communication with the families but also among the professionals, since a lack of communication is the cause of a high percentage of errors.17
InterventionDuring the month of February we held sessions in communication skills, decision making and the limitation of life support, together with coaching sessions and professional motivation initiatives conducted by specialized psychologists. Relaxation techniques such as Reiki and craniosacral therapy were imparted. In this monthly commitment we participated in a session focused on “self-counseling” or the set of skills needed for relating to oneself and to others, with the purpose of improving the physical, emotional and spiritual health of the professionals and gain awareness of the need to acquire self-help and personal growth skills or strategies. In sum, emotional, social and motivational gymnastics.18
In another session, involving taped real-life testimonies of the relatives of patients admitted to the ICU, we highlighted the demand for information on the part of the families, revealing the communication deficiencies we have with them and among ourselves as professionals.
4. March: Breaking barriers, greater accompaniment: the open doors H-ICUBackground“Open ICUs” are Units that seek to reduce or suppress imposed time, physical or relational limitations for which there is no justification.
Much has been written about the strictness of visiting hours in our ICUs – this being one of the main concerns of the patients and their families. The “family resource” is a key element for the control of anxiety and delirium in the ICU. In this regard, families demand more time and flexibility with the visiting hours.19,20 Despite the fact that many studies recommend a more open policy and associate healthcare outcomes to the organizational system, the presence of protocols, multidisciplinary teamwork and efficient resource utilization – including the visiting policy21–23 – the fact is that most ICUs are restrictive. In Spain, 67.7% of our Units continue to limit visits to twice a day, and only 4% have a 24-h open policy.20 Similar situations are found in the rest of Europe.23–25
Restricted visiting hours are assumed because professionals feel that “the natural place of the family is outside the Unit”, and in some instances allowing or not allowing visits is seen as an instrument of power or as a means of reward/punishment, depending on the behavior of the relatives.26
The families demand security and confidence from the healthcare professionals.27 It does not seem logical to expect them to trust us or value our work if they are left outside the Unit for at least 20h a day.25,26
This is one of the most difficult barriers to overcome. Healthcare professionals feel the nearby presence of the relatives to be an added source of stress. In this regard, we must start with the important change in mentality required and the change in working dynamics implied. Progressive effort is needed, “first opening minds and then doors”.20
InterventionIn the ICU of Infanta Margarita Hospital we conducted a survey among the professionals of the Unit in order to know their opinion (Fig. 2 of Annex 1. Supplementary material). The initiative was launched under the title: “Opening the Intensive Care Unit to the families: what do the professionals think?”, and had the following objectives:
- •
To assess agreement/disagreement with the proposal to expand the visiting hours.
- •
To encourage contributions and identify room for improvement.
- •
To know the possible barriers facing the implementation of such measures.
Sixty-four percent of the staff members that answered the questionnaire were in favor of a more open ICU, and numerous suggestions and options for improving the proposal were recorded.
Debate was held in a joint session, and consensus was reached to adopt a concrete expanded visiting model in our Unit. We chose a model of three visits a day, with the possibility of interchanging relatives, and expanded up until mealtimes. Family accompaniment throughout the afternoon and until midnight was offered, and information or visits in other time intervals was personalized if so required by the particular circumstances of the family. On occasion of the morning round, the nurse identified the family situation and recorded it in writing on the daily round checklist or on the patient care schedule; based on these data, the type and time of accompaniment was then decided (hours, reference relatives).
An internal document was drafted to ensure correct functioning of the new non-restrictive visiting policy and to define the role to be played by each member of the team. An informative letter for the families was also produced.
ResultsSince the start of the project and our organization based on a “more open” ICU, we have standardized the coming of families to the nursing controls, speaking with the professionals, collaborating in care or accompanying the patient. Likewise, we have standardized personalization and adaptation of the visit information hours to the family needs. In our experience, rather than a source of problems or alterations, the family has been a resource in our favor, offering help and alliance in our work. In contrast to what could have been expected, the families do not demand much more attention, and they trust the team more, since they see how we care for and attend their ill relatives. We are continuously receiving more thanks and recognition from both the healthcare professionals of our area and from the families, and this encourages us to remain motivated in our work. They know us better, they value us more, and they trust us more.
5. April: The H-ICU comes out of the ICU; we are people that care for people. Citizen information campaignBackgroundEach year the professionals of the ICU of Infanta Margarita Hospital organize courses for nursing staff, residents in training or staff physicians. With this commitment our aim was to approach other non-healthcare collectivities in the hope of explaining our work and our specialty a little more in detail.
InterventionIn this month we conducted an informative campaign targeted to citizens, leaving our hospital setting, with the organization of a series of sessions: “The ICU is LIFE”. With this initiative we came into contact with the population, in out-hospital facilities, supported by the local city authorities, training citizens to recognize and ensure prompt intervention in the main time-dependent disease emergencies. Activities were also targeted to different associations, and we moreover established a training agreement for first intervening individuals such as firemen in the zone or the sociosanitary staff of a home for disabled people–thereby making our dimension as trainers better known. These training activities are repeated on a regular basis, addressing different topics each time, according to an established plan, and agreed with the different associations.
6. May: Sharing experiences: meetings with families and between familiesBackgroundWe considered it necessary to create a space for listening, allowing us to truly understand the experiences of others and create better communication routes, assimilating the needs of the patients and their families, and forming a joint patient-family care unit.
InterventionWe dedicated the month of May to meets with several families of ICU survivors, sharing their experiences with them.
The meets were organized by a group of nurses, with the selection of a focal group of families that were contacted by telephone. The meets were held outside the ICU setting, in facilities offered by the local city authorities. By leaving our natural habitat (the walls of the ICU), we crossed a barrier to “expose ourselves”, free from professional conditionings, and were able to interact with the families in a more natural way.
ResultsThe experience was very gratifying. Their direct testimonies made us more aware of the feelings, needs and lacks experienced by the families during the intense period in the ICU.
A pending issue is the organization of similar meets with the families of patients that died in the Unit.
7. June: Another little step: enjoy the scenery. We bring the patients out of the ICU boxes; we have some wonderful window viewsBackgroundThe mood state of patients admitted to the ICU is strongly influenced by the surroundings. Adequate illumination helps maintain the biological clocks and serves as an orienting element for patients. Scenery also forms part of what is regarded as a humanized infrastructure.5
InterventionTaking advantage of our ample and well illuminated facilities, we developed a nursing-guided protocol for selected patients that could benefit from leaving the rooms (boxes). The necessary safety measures (monitoring, supportive devices) were adopted, with the simple purpose of moving the patients to the windows or covering a few meters toward the family waiting room. In a group of selected cases, such as coronary patients, we even offered the possibility of going accompanied to the bathroom. The implication of the accessory staff of the Unit was essential in this intervention.
8. July: We continue breaking barriers: the families enter the H-ICU to collaborate in patient care, hygiene, etc.BackgroundWe advanced in the “use” of the families as a care “resource”, not only due to the benefits for the patients, but also because admission to the ICU is a traumatic experience for families, causing great frustration, and they feel the need to contribute in some way–such as for example participating in some patient care routines. Another benefit of this practice is that the relatives can become familiarized with the care measures the patient may need after discharge from the ICU (management of tracheostomized patients, etc.).28 We not only offer families the opportunity to feel useful, but moreover also show them our work: what is being done in the Unit during those never-ending hours they spend in the waiting rooms.19 Some nursing societies, such as the Andalusian Society, already have established recommendations for integrating family participation in patient hygiene, physiotherapy, etc.29
InterventionThis commitment was characterized by considerable controversy among the nursing assistants. In some cases, they did “not feel comfortable” performing measures of hygiene in the presence of the family, while in other cases the opinion was that the family is “not prepared” for such tasks. The meetings of the working groups allowed flexibilization, discussion and the individualization of cases.
Our ICU developed a protocol called “Caring for my relative”, in which the families were offered the opportunity to participate in activities referred to patient hygiene, meals, mobilization or the learning of certain physiotherapy exercises. A satisfaction questionnaire targeted to the families that have participated in such activities has also been implemented and is pending analysis.
9. August: Technologies for the patients: TV, mobile phone, Facebook… why not?BackgroundWe live connected, we communicate, relate, inform and entertain ourselves with these technologies. Patients who are in a clinical condition allowing them to do so, and who wish to remain connected to their daily life routines, should be offered the chance to use such technologies. We may need less sedation if the patient is able to stay connected to the outside, to friends and relatives, thanks to the new technologies. According to different studies, most ICU rooms have no access to a telephone, no clock with the time and date, no radio, etc.9,19
Facilitating patient distraction and communication forms part of a humanized structure.5
InterventionThis monthly commitment was dedicated to securing improved technological resources. A formal request was submitted to the Hospital Management for a wifi network, television, clocks with the time and date for the rooms, an increased presence of DVD devices and music players. Most of these petitions remain to be completed.
Private donations have yielded mp3 and mp4 players and several DVD devices, allowing us to organize a video library covering a broad range of choices. Patients are allowed to freely use mobile phones, tablets, computers and other devices with the purpose of remaining connected to their personal environment.
10. September: Respect for patient intimacy: a priority in the H-ICUIn the 2014, and coinciding with the organization of a regional congress in Intensive Care Medicine, we presented a series of strategies to strictly protect the intimacy of our patients.
A list of good practice principles was produced to guarantee the intimacy of the critical patient, and posters were distributed on the walls of our Unit in order to always keep these principles in mind during our daily activities:
- -
Respect for body intimacy: we ask for permission to undress, touch and explore the patient, with a prior explanation of what is going to be done. Special gentleness is observed during personal hygiene.
- -
Respect for physical space: the box is kept closed if so preferred by the patient, letting him or her know who is going to enter and what for.
- -
Collection of information about the patient: we ask only what is necessary; we are not legitimized to ask anything we wish.
- -
Information shared with other team members caring for the patient: we decide what information is to be transmitted to the team and what information that should be kept to oneself, in those cases where the information affords no benefit for the clinical process and might violate patient intimacy.
- -
Telephone-delivered information: no clinical information is delivered by telephone, apart from exceptional cases and with guarantees of knowing who we are speaking with. Express consent of the patient is moreover required.
- -
Respect for the intimacy and participation of the family or related persons: we ask the patient who he or she wishes to be informed, since it is a patient right to choose with whom personal health information can be shared with. Adulthood in healthcare is 16 years, and at this age the patient has the right to confidentiality and to information of a personal nature.
- -
Custody of the clinical history: the clinical history is to be kept safely to prevent any undesired violation of patient intimacy.
- -
Intimacy on receiving visits during admission: patients have the right to decide who can visit them. Attempts are to be made to improve patient appearance when receiving a visit, in order to help improve self-esteem.
- -
Intimacy in transfer for complementary tests or to other areas of the hospital: care is required, paying attention to physical exposure during patient transfer.
- -
Respect for the public and social image of the patient: information is not to be delivered to the media (accidents, aggression, public persons, etc.), unless prior authorization has been given.
The main objective of Intensive Care Medicine is to reduce morbidity-mortality, as well as to maintain or improve the functional capacity and quality of life of our patients. The objective of a patient admitted to the ICU is to return to his or her previous health condition, or to a situation that can be reasonably expected in a person of the same age group and medical situation. Posttraumatic stress disorder (PTSD) is a type of anxiety disorder that develops following a highly traumatic event involving an extreme life-threatening situation.30
Surviving serious illness is a traumatic experience that can give rise to PTSD. Starting from 3–5 days after admission to the ICU, many patients suffer anxiety and depression.31 Such problems have been reported in up to 20% of all patients admitted to Intensive Care.32
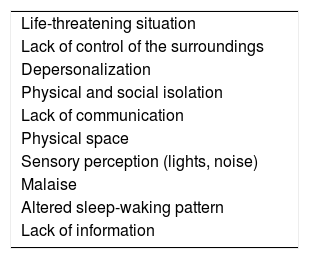
Patient vulnerability is related to extreme emotional and physical dependency (Table 1).
Posttraumatic stress disorder is therefore a complication following admission to the ICU and which along with comorbidity associated to depressive disorders (60–80%) has a strong impact upon the health-related quality of life of patients at the time of discharge. Depression and anxiety symptoms develop in 8–57% and 23–48% of patients, respectively. Less than 10% of all patients subjected to mechanical ventilation for more than four days are still alive and fully independent after one year.33
While admission to the ICU produces anxiety, discharge from the Unit causes fear, also in the family, with a sense of helplessness and loss of security. This in turn again produces a stress response and confusion, leading to physical and emotional exhaustion. In effect, the family also suffers stress and anxiety, sometimes resulting in the exacerbation of previous disease conditions or the need for antidepressive medication. Family dynamics become destabilized.
The prevention of these problems is complex, and involves a series of interventions that implicate all the care team members.
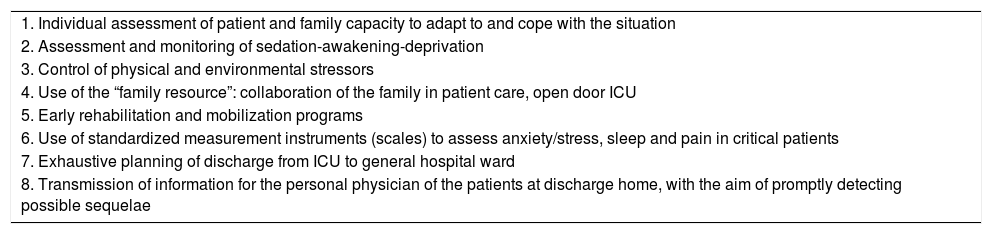
We started to work in this field in 2014, and proposed 8 opportunities for improvement with a view to preventing and/or detecting PTSD (Table 2).
Opportunities for improvement in the prevention of posttraumatic stress disorder.
| 1. Individual assessment of patient and family capacity to adapt to and cope with the situation |
| 2. Assessment and monitoring of sedation-awakening-deprivation |
| 3. Control of physical and environmental stressors |
| 4. Use of the “family resource”: collaboration of the family in patient care, open door ICU |
| 5. Early rehabilitation and mobilization programs |
| 6. Use of standardized measurement instruments (scales) to assess anxiety/stress, sleep and pain in critical patients |
| 7. Exhaustive planning of discharge from ICU to general hospital ward |
| 8. Transmission of information for the personal physician of the patients at discharge home, with the aim of promptly detecting possible sequelae |
During the development of our project, a working group was established with the following activities:
- 1.
Literature review, affording a context an justification of PTSD.
- 2.
Informative clinical sessions involving all staff members of the Unit, with an analysis of both the physical and the psychological stressors. Noise is regarded as one of the main physical stressors, and in this context the ICU is a constant source of noise generated by both medical equipment and staff.34 Excessive levels produce stress and delirium, and have a wearing effect upon the healthcare professionals. Other physical stressors are pain, the presence of tubes, incapacity to communicate, fear, or a lack of control upon oneself.35
- 3.
Development of a nursing-guided protocol describing the measures to be adopted in order to prevent PTSD.
- 4.
A qualitative study was made, involving an open, individual and semistructured interview of a focal group of patients, designed to document their experiences. A sample of long-stay (over 30 days) patients admitted to our Unit between January 2010 and October 2016 was selected and contacted by telephone. The survey was carried out in the setting chosen by the patients – in this case the home. The interview sought to evaluate memory of stay in the Unit, physical and psychological stressors, sequelae, and post-ICU syndrome.
We learned about the experience of the patients, addressing not only “how many” stressors they suffered but also the “what”, “how” and “why”, from their perspective and that of their relatives. We explored their memories, with findings very similar to those reported by other authors.36
This work was subsequently presented during a clinical session, giving us an opportunity for reflection as a team and for analyzing our work from another point of view.
The next step comprises implementation of the protocol proposed by the nursing staff for the early detection and prevention of PTSD.
12. November: An H-ICU for all. What you think is important for us: satisfaction questionnaires, ideas and suggestions for professionals of the rest of the Hospital, relatives and patientsBackgroundTo date, we have carried out our commitments each month, living them from our ICU and transmitting them within our own Hospital and among the colleagues of other nearby Hospitals through personal contact, the media, and especially the social networks from our Facebook page: Project ICU Infanta Margarita Hospital: 1 year: 12 months for 12 commitments.6 Thanks to this resource it has been possible to go much further than we ever believed possible.
We considered it mandatory to know the opinion of our surroundings, professionals and relatives.
InterventionDuring the month of November, we conducted a structured survey of the professionals of the Hospital and the healthcare area (Fig. 3 of Annex 1. Supplementary material) with the purpose not only of evaluating the project but also of exploring opinions about the professionals and the ICU.
We likewise resumed another survey that had already been developed to know the opinion of the relatives of patients admitted to the ICU (Fig. 4 of Annex 1. Supplementary material). In this commitment we aimed to continue exploring the family needs. Most studies indicate that families fundamentally demand information, security, wellbeing, support and closeness to the patient.26,37 The survey is administered at patient discharge from the Unit, along with the report, explaining to the family that they can place it at any time in a booth located at the entrance to the Unit. Most families deliver it in some moment during patient admission to the hospital ward.
Both surveys are pending evaluation.
Future actionsOur intention in the present initiative–Project ICU Infanta Margarita Hospital: 1 year: 12 months for 12 commitments–has been to work upon most of the aspects embodied within the concept of humanization: the professional, the family, infrastructure, the patients and their way of life, communication and respect for personal decision. Most of the experiences published in the literature focus on some of our commitments in an isolated manner only, and we feel that our project has been a considerably more complete. The Plan for Humanization of the ICU in the Community of Madrid was published in 2016, and reflects many of the lines and recommendations on which we have been working.4
In our opinion, the main strengths allowing us to fully implement the project have been:
The monthly public commitment we made from the start with our Hospital and our community.
Organization, with clear identification of the leader and of the working groups.
Broad diffusion of the project in the media, continuously making us feel responsible for continuing the project, and which offered us positive feedback.
The fact that ours is a small and highly cohesive ICU has also been a favoring element.
The future challenges in relation to what we presently perceive as weaknesses or pending issues are:
Training in communication tools.
The development of motivation strategies for professionals.
Progression in topics as novel as music therapy, which requires something more than voluntary participation of the music therapist in the project.
Analysis of the surveys of the healthcare professionals in our setting and of the families, assuming criticisms and launching plans for improvement.
Attempts to obtain help for completing some commitments that require funding and which do not depend on the Unit itself (training courses, the acquisition of material for music therapy, grants, television sets, clocks). This is a very slow process, and many of these aspects remain pending.
The coming year we intend to consolidate the results obtained and continue to work especially upon measures for the prevention of PTSD, with a prospective study that is already underway.
We continue working on the open ICU and have developed a new questionnaire for the professionals of the Unit (Fig. 5 of Annex 1. Supplementary material), with the aim of knowing their opinion–one year later–about the impact of the expansion of visiting hours and establishing comparisons with the opinion at the start of the project.
Lastly, it must be underscored that the humanization of healthcare is so current and timeless that it belongs to always and now. As professionals we must show respect to ourselves and to others, and promote among us values such as sensitivity, solidarity, generosity and empathy, active listening, respect and compassion,2 among other qualities. Far from making us weaker, these should be increasingly valued qualities.
Humanization programs in Intensive Care should be individualized for each setting, Unit and team. Each group of professionals should analyze its barriers and difficulties, and determine how far it wishes or is able to go. Good organization is essential, with the implication of as many members as possible, making them feel as active participants in this great change.
Our project has been supported by enormous solidarity and generosity. However, it must not be forgotten that in order to humanize, the most important elements are the human resources, and that humanization plans not only need voluntary acts and private initiatives but also investment in the number and care of professionals, materials and infrastructure–because we are at risk of suffering intense wear and of falling short of our objectives. Explicit commitment on the part of the health institutions is therefore essential.
Financial supportThe authors declare that they have received no external financial support.
Conflict of interestThe authors declare that they have no conflicts of interest.
Thanks are due to the generosity of the professionals of the ICU of Infanta Margarita Hospital.
Please cite this article as: de la Fuente-Martos C, Rojas-Amezcua M, Gómez-Espejo MR, Lara-Aguayo P, Morán-Fernandez E, Aguilar-Alonso E. Implantación de un proyecto de humanización en una Unidad de Cuidados Intensivos. Med Intensiva. 2018;42:99–109.