Traditionally, the goal of intensive medicine has been to reduce short-term mortality yet, today, the management of critically ill patients should focus on goals that go far beyond survival. It is estimated that, at least, half of the survivors of critical conditions will end up showing symptoms associated with the post-intensive care syndrome (PICS)–an entity including health issues that the patient displays after leaving the critical condition such as psychiatric, cognitive, and physical disorders. The risk factors vary based on the area of the PICS element studied1 (Table 1).
Post-intensive care syndrome. Description, risk factors, and natural history.
| Complication | Description | Risk factors | Natural history |
|---|---|---|---|
| Physical function | Impairment of ADL | Sepsis. ARDS. MV>7 days. MODS. Poor glucose regulation. Age. Vasoactive drugs. Corticosteroids. | Improvement of ADL in a matter of months |
| Pulmonary function | Impaired spirometry, lung volumes and diffusing capacity | Duration of MV | Usually mild during the first year, but it can remain for another five years |
| Psychiatric | 1. Depression | Sepsis, ARDS, trauma, hypoglycemia, hypoxemia, delusional memories. Sedation, former unemployment. | 1. Depression: It can improve during the first year |
| 2. Anxiety | 2. Anxiety: It can remain beyond the first year | ||
| 3. PTSD | Women, Age <50 years old. Alcoholism. | 3. PTSD: Poor improvement during the first year | |
| Cognitive | Memory disorder. Attention. Executive function. Speed of mental processing. Visual-spatial ability | Delirium | Significant improvement during the first year. Residual deficit up to six years |
| Sepsis | |||
| ARDS | |||
| Other (glucose dysregulation, duration of MV, hypotension, CRA, …) |
ADL: Activities of daily living. ARDS: Acute Respiratory Distress Syndrome. MODS: Multiple organ dysfunction syndrome. MV: Mechanical ventilation. PTSD: Post-traumatic stress disorder. CRA: Cardiorespiratory arrest.
PICS-associated psychiatric disorders include post-traumatic stress disorders (PTSD), anxiety, and depression. PTSD is associated with terrifying experiences during ICU stays. The symptoms consistent with PTSD occur in one (1) out of every five (5) survivors of critical conditions twelve (12) months after their ICU stay, and there is a higher prevalence in patients with a psychiatric history who experienced memories during their ICU stay and received benzodiazepines, although in this last case, the causal relation cannot be established.2
Acute respiratory distress syndrome (ARDS) survivors experience frequent psychiatric disorders after their ICU stay. It has been confirmed that 36 per cent, 42 per cent, and 24 per cent of these patients show symptoms of depression, anxiety, and PTSD, respectively, some six (6) months after being discharged from the hospital, with minimum changes of prevalence at 12 months. Being of a younger age was associated with anxiety and PTSD, while longer courses of opioid treatment were associated with symptoms of depression, and anxiety.3
Cognitive disordersCognitive disorders damage the executive function, memory, and attention. The delirium is an independent risk factor for its development. The global cognition and executive function assessment of one cohort of patients with acute respiratory distress; cardiogenic shock; or septic shock confirmed that three (3) months after being discharged from the hospital, 40 per cent of the patients had a below average global cognitive score of 1.5 standard deviations, while 26 per cent of the patients had a below average global cognitive score of 2 standard deviations (similar to that of patients with mild Alzheimer's disease). The annual figures were 34 per cent, and 24 per cent, respectively. Longer bouts of delirium were associated with worse cognition and executive function at 3 and 12 months, respectively. High doses of benzodiazepines were not associated with worse long-term cognitive scores, but they were an independent risk factor of worse executive function scores at 3 months.4
Physical disordersMobility-limiting physical disorders are very common in the early stages of the post-ICU period. Most patients, especially those who have had long stays at the ICU, are not self-sufficient patients during the first week after hospital discharge.5 Functional independence improves with early rehabilitation programs, but regaining muscle mass and strength can take weeks, months or even years after hospital discharge.6 Recently, muscle weakness measured using the Clinical Frailty Score has been associated with higher mortality rates at 3 and 12 months.7
ICU-acquired muscle weakness is a clinical diagnosis. The typical presentation in the acute phase is symmetric muscle weakness that affects the limbs and respiratory muscles. Terms such as polyneuropathy; myopathy in critically ill patients; or neuromyopathy speak to us about the underlying condition and are identified through neurophysiology or muscle biopsy. Not all patients with ICU-acquired muscle weakness show polyneuropathy or critical illness myopathy. Not all patients with a neurophysiological diagnosis of neuropathy or myopathy have ICU-acquired muscle weakness, even though the risk of developing it is high. Among the physiopathological findings, the calpain and ubiquitine-proteasome mediated myofibrillar protein rupture is one of the key elements, especially during the sepsis, that leads to a loss of myosin filaments; sarcomere disassembly; and muscle dystrophy. This increase in the rate of muscle protein ruptures gets worse with immobilization which, to a greater or lesser extent, is one of the constants of critically ill patients.8
The office of intensive outpatient careThe identification and management of the PICS requires one multidisciplinary team.
Since 2009, the guidelines published by the U.K. National Health Service through its National Institute for Health and Care Excellence recommends all its hospitals to review the provision of follow-up units for critically ill patients.9
In our country, the Hospital Universitario La Paz Critical Care Medicine Department (CCMD) has started a program for PICS detection and follow-up. Without leaving out the strategies aimed at its prevention,10 the elements of the project focus on the follow-ups conducted at the hospital floors and the check-ups conducted at the office of intensive outpatient care of patients at risk of developing PICS.
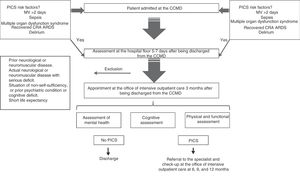
The patient at risk is assessed at the hospital floor 5–7 days after being discharged from the CCMD, and should he still be eligible for assessment, a new appointment is arranged three (3) months later at the office of intensive outpatient care. The actions that will be conducted there are: anamnesis from the moment of hospital discharge; physical examination; assessment of pulmonary function; assessment of muscle strength; functional assessment; and quality of life, psychological and cognitive assessments. Based on the characteristics of the patients, a new appointment will be arranged with each individual 6, 9 and 12 months later or, in the absence of alterations requiring further medical appointments, the patient will be discharged from the hospital. Additionally, based on the alterations found, the patients can be referred to the corresponding medical specialists (Fig. 1). The CCMD teams up with the unit of psychiatry and the rehab unit for the implementation of this program.
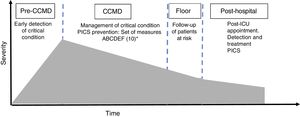
The conceptual changes of our medical specialty have brought the intensivist out of the CCMD. Following in the footsteps of this philosophy, the project aims at providing better healthcare to the critically ill patient before, during, and “after” the resolution of his critical condition11 (Fig. 2). Therefore, the answer to the question posed at the beginning of this point of view letter is affirmative. One multidisciplinary team coordinated by the intensivist, who has been following the clinical trajectory of the patient during his stay at the CCMD, is the strategy that should be followed in order to achieve the final goal of intensive medicine, that is, bring back the patient to his activities of daily living–both professional and socially in optimal health conditions both physically and mentally.
Model of critical condition. Edited by Angus and Carlet.11 CCMD: critical care medicine department. a Set of prevention measures ‘ABCDEF’: (A) prevention and management of pain; (B) sedative withdrawal test. Spontaneous breathing trial; (C) choice of analgesia and sedation; (D) prevention and management of delirium; (E) early mobilization; and (F) involvement of the families.
The authors declare that they have no conflicts of interest whatsoever.
Please cite this article as: Extremera P, Añón JM, García de Lorenzo A. ¿Están justificadas las consultas externas de medicina intensiva? Med Intensiva. 2018;42:110–113.