To analyze the incidents related to patient safety (IRSP) and their risk factors during in-hospital transfer (IHT) of critical patients after the application of a protocol, and to evaluate safety during transfer using quality indicators.
DesignA prospective, observational and non-intervention cohort study was carried out.
SettingA 10-bed multipurpose Intensive Care Unit (ICU) of a second level university hospital.
PatientsAll IHTs of critical patients in the ICU for diagnostic tests and to the operating room between March 2011 and March 2017 were included in the study.
Main measurementsDemographic variables, patient severity, transfer priority, moment of the day, reason and type of transfer team. Pre-transport checklist items and IRSP were collected. A biannual analysis was made of quality indicators designed for IHT.
ResultsA total of 805 transfers were registered, mostly of an urgent nature (53.7%) and for diagnostic tests (77%). In turn, 112 transfers (13.9%) presented some type of IRSP; 54% related to the equipment and 30% related to team and organization. Adverse events occurred in 19 (2.4%) transfers. Risk factors identified in the multivariate analysis were mechanical ventilation and the transport team. The evolution of the indicators related to transport was significantly favorable.
ConclusionsAfter the application of an IHT protocol, IRSP are low. The main risk factor is invasive mechanical ventilation. The experience of the team performing IHT influences the detection of a greater number of incidents.
Analizar los incidentes relacionados con la seguridad del paciente (IRSP) durante los traslados intrahospitalarios (TIH) del paciente crítico tras la aplicación de un protocolo, así como sus factores de riesgo. Evaluar la seguridad durante los traslados mediante indicadores de calidad.
DiseñoEstudio de cohorte, prospectivo, observacional y no intervencionista.
ÁmbitoUnidad de Cuidados Intensivos (UCI) polivalente de 10 camas de un hospital universitario de segundo nivel.
PacientesSe incluyen todos los TIH de pacientes críticos realizados de UCI a pruebas diagnósticas y a quirófano entre marzo de 2011 y marzo de 2017.
Principales variables del estudioVariables demográficas, gravedad de los pacientes, prioridad del traslado, momento del día, motivo y tipo de equipo del traslado. Se recogen comprobaciones pre-traslado e IRSP. Análisis semestral de indicadores de calidad diseñados para el TIH.
ResultadosDe los 805 traslados registrados, la mayoría urgentes (53,7%) y para pruebas diagnósticas (77%), 112 traslados (13,9%) presentaron algún tipo de IRSP, 54% relacionado con el equipamiento y 30% con el equipo y la organización. En 19 (2,4%) traslados se produjeron eventos adversos. En el análisis multivariante los factores de riesgo fueron la ventilación mecánica y el equipo que realiza el traslado. La evolución de los indicadores relacionados con los traslados es significativamente favorable.
ConclusionesTras la aplicación de un protocolo de TIH, los IRSP son bajos y el principal factor de riesgo es la ventilación mecánica invasiva. La experiencia del equipo que realiza el TIH influye en la detección de un mayor número de incidentes.
The intensive care unit (ICU) is a space where healthcare is provided and where numerous patients safety incidents (PSI) can occur.1 In the study conducted by the Spanish Society for Intensive Medicine, Critical Care and Coronary Units on the critically ill patient safety and risk (CIPSR) a minimum of 6 incidents per 100 patients were reported at the 1 -h follow-up.2 The most common contributing factors were associated with those critically ill patients especially vulnerable due to the inherent severity of their condition.3
PSI are considered adverse events (AE) if they hurt the patient or harmless incidents (HI) if they don’t or if they don’t have negative consequences for the patient.4
In-hospital transfer (IHT) is a common procedure at the ICU setting to perform diagnostic tests or therapeutic procedures.5 Critically ill patients who need to be transferred outside the ICU have a significantly higher risk of AE.6 Also, invasive mechanical ventilation (IMV) increases the risk of PSI during the transfer.7–11
Different epidemiological studies have contributed to knowing IHT-related EA. They have also helped us be able to identify risk factors like patient’s severity, the organization of the transfer, equipment-related technical factors, and human factors of the healthcare team doing the transfer.5,12,13 Some of them increase the chances of serious incidents occurring like emergency transfers, the need for catecholamines in continuous perfusion due to hemodynamic instability, and IMV.14 The overall rate of AE during the IHT of the critically ill patient is between 1.7% and 76%.8,15The associated mortality rate is 2% according to the different series described.8,9
Different clinical practice guidelines on the management of IHT, and specific protocols on how to standardize care, equipment, the training of the healthcare team, and the degree of experience required to increase safety have already been published; also, checklists of drugs and materials needed to mitigate PSI.5,12,13,16–18 Also, the transfer of information is one key aspect we should consider if we wish to increase the safety of critically ill patients;19 however, the rate of AE is still high.8,15
The objective of this study was to analyze IHT after the implementation of an IHT protocol for the critically ill patient to perform diagnostic tests or transfers to our ICU operating room. Also, to know the rate of PSI, risk factors, and the impact in time that improvement actions have through assessments every 6 months of the quality indicators associated with the safety of IHT.
Patients and methodsObservational, prospective study at the ICU of a level II hospital with 10 polyvalent beds. Inclusion criteria: all IHTs of critically ill patients performed from the ICU to run diagnostic tests or surgical room transfers between March 2011 through March 2017. Other IHTs of critically ill patients inside the hospital were excluded.
The following variables were studied: transfer priority (emergency or scheduled), time of the day, reason for the transfer (to run diagnostic tests or transfer the patient to the surgical room), composition and experience of the transfer team, demographic data, and the APACHE II (Acute Physiology and Chronic Health Evaluation II) score of every patient. The following protocol was used in all the transfers: run a previous checklist to confirm hemodynamic, neurological, and respiratory stability; check the airway, necessary perfusions, and drainages; double check all the necessary material and drugs; prepare the stretcher for the transfer, portable ventilator, monitor/defibrillator, and oxygen supply; patient-dependent planning by the healthcare team, and coordinator with the recipient team.
The IHT team was organized based on the patient’s status. Patients without vasoactive drugs (VAD), in spontaneous breathing, and without neurological disorders were transferred by the nursing staff and the unit orderly. Patients with VAD and/or neurological disorders, but still in spontaneous breathing were transferred by the treating doctor or nurse plus the orderly. Patients with VAD and IMV were transferred by the treating doctor or nurse, the orderly, and a second nurse. Also, the safety experience of the doctor who handled the IHT was analyzed, that is, whether he had been trained in safety issues regarding patient safety and risk management at the ICU setting.
Once every IHT had been completed, it was included in an electronic registry with all the variables studied, all the checklists run, and with all the PSI that had occurred during the transfer.
PSI were defined as events or circumstances that may have caused or did cause unnecessary damage to the patient. They were considered as a HI if they never hurt the patient because they never actually reached him or if they did, they never had any consequences for him. AE were defined as those events that ended up hurting the patient resulting in physiological, although transient, impairment, that may have triggered death, residual inability at discharge or that required performing a certain procedure. Contributing factors were defined as all those circumstances, actions or influences that played a role in the origin and development of an AE.4 In order to stratify the severity of the PSI, an adaptation of the Classification Scheme for Medication Errors designed by Ruiz-Jarabo et al. was used.20
Data from the electronic registry of all IHTs performed were analyzed every 6 months, as well as the degree of compliance with the checklists run before the transfer, the PSI found, and all the associated risk factors.
The following quality indicators were designed: “IHT with PSI” (number of transfers with PSI/total number of transfers × 100), and “IHT with AE” (number of transfers with AE/total number of transfers × 100). The biannual study of these indicators allowed us to implement improvement actions that would be gradually implemented across time and throughout the study period.
The use of the electronic registries of the IHTs of ICU-based critically ill patients was approved by the Fundació d’Osona per a la Recerca i l’Educació Sanitàries (FORES) of the Consorcio Hospitalario de Vic research ethics committee. This was an observational, non-procedural study whose registry of patients has enough guarantees for data protection, which is why it wasn’t considered necessary to request the patients’ informed consent.
The SPSS Statistics 23 statistical software package was used. Qualitative variables were expressed as frequencies and percentages. Quantitative variables with normal distribution were expressed as mean and standard deviation. Those without a normal distribution were expressed as median, minimum, and maximum. To analyze the risk factors of PSI associated with IHT, a bivariate analysis was conducted including contingency tables, the chi-square test for categorical variables, a comparison of means, and the Student t test or the non-parametric Mann–Whitney U test for the quantitative variables. A multivariate logistic regression analysis was performed. Statistical significance was set at 5%.
ResultsA total of 805 IHTs of 418 patients were performed between March 2011 through March 2017. Most were emergency transfers: 432 (53.7%). The reason for 77.1% of these transfers was to perform diagnostic tests, 19.5% to perform surgical procedures, and 3.4% for other reasons. A total of 40% of the patients required more than 1 transfer during their ICU stay. Most transfers [81% (653)] occurred during the morning shift. The mean age of the patients transferred was 62.7 ± 14 years. A total of 72.2% were men, and the mean APACHE II score was 19 ± 7 (between 0 and 53). The median ICU stay was long [18 days (minimum, 1; maximum, 136)]. The mortality rate of the 418 patients was 14.4%.
A total of 60% of the patients transferred were surgical patients, and in 60% the reason for ICU admission was sepsis/septic shock. In 366 transfers (45.5%) the patient remained on IMV.
The IHT team included the treating doctor and nurse plus another assistant nurse and orderly in patients with VAD and IMV. In 486 IHTs (60.4%) it was the treating doctor, the nurse, and the orderly who were responsible for the patient, and in 27 IHTs (3.4%) only the nurse and the orderly.
Regarding the experience of the intensivist doing the transfer, in 220 IHTs (27.3%) these were senior experts in safety issues, 437 (54,3%) were seniors, and 121 (15%) were doctors on call. Critically ill patients transferred by expert doctors in safety issues were in a more critical condition (APACHE II = 21.2 ± 6.1) (P < .001), and more of them were on IMV (48.6%, non-statistically significant P = .3).
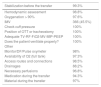
Compliance with the checklist before the transfer was very high (Table 1).
Checklist before in-hospital transfer.
| Stabilization before the transfer | 99.3% |
|---|---|
| Hemodynamic assessment | 98.8% |
| Oxygenation > 90% | 97.6% |
| IMV | 366 (45.5%) |
| Check cuff pressure | 100% |
| Position of OTT or tracheostomy | 100% |
| Adequate TV-RF-FiO2-MV-MIP-PEEP | 100% |
| Does the patient ventilate properly? | 100% |
| Other | |
| Monitor/DF/Pulse oxymeter | 98% |
| Availability of O2 (full tank) | 97.3% |
| Access routes and connections | 98.5% |
| Drainages | 88.2% |
| Necessary perfusions | 96.8% |
| Medication during the transfer | 94.3% |
| Material during the transfer | 97% |
A total of 112 transfers had PSI (13.9%) but 693 transfers didn’t (86.1%). In 93 transfers (83%), a total of 136 His were reported, and in 19 transfers (17%) AE were reported (2.4% of the total number of IHTs performed). No IHT-related deaths were reported.
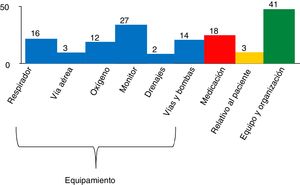
A total of 54.5% of all PSI had to do with the equipment, 30% with the transfer team and organization, 13.2% with a lack of drugs or material for the transfer, and 2.2% with the patient’s critical condition (Fig. 1). AE were specifically described on 16 occasions and all of them required a procedure; 47% due to hemodynamic alterations, 33% due to respiratory conditions, and 20% due to other causes. The most common ones were arterial hypotension and desaturation that required intubation in 1 patient during the IHT. A total of 6 AE were considered serious.20 On 3 different occasions the AE that had occurred was not specifically described (Table 2).
Description of adverse events.
| Adverse event | |
|---|---|
| Unreported | 3 |
| Contrast-induced vomits through the NGT | 1 |
| Transient asystole due to transcutaneous pacemaker disconnection | 1 |
| Hypertensive crisis and arrhythmias* | 1 |
| Desaturation | 2 |
| Prosthetic hip dislocation* | 1 |
| Sedation-induced arterial hypotension | 2 |
| Hypoxemia and extreme bradycardia* | 1 |
| Hemodynamic instability* | 1 |
| Intubation due to desaturation, acute respiratory failure* | 1 |
| Arterial hypotension due to failed pumps | 1 |
| Hyperventilation in neurocritical patient during MRI (manual ventilation with self-inflatable bag) | 1 |
| Massive pneumothorax* | 1 |
| Bradycardia | 1 |
| Renal function impairment due contrast nephropathy (repetition of abdominal CT due to technical difficulties) | 1 |
The finding of PSI during the transfer was significantly associated with the appearance of AE (P < .001). In 18 IHTs a total of 26 incidents considered contributing factors for the appearance of AE were identified. The most common problems were associated with the portable ventilator or oxygen (46%) and with disorders due to the severity of the patient’s condition (19%).
No significant differences were seen when the IHTs where PSI were found were compared to the IHTs where no PSI were found regarding age, sex, priority, shift or reason for IHT (Table 3). The IHTs performed within the first 48 hours after ICU admission, when the patient is supposed to be more unstable, did not have any more PSI compared to the IHTs performed after the first 48 hours after ICU admission. No differences were found either in the days on IMV or in the mortality rate 28, 60 or 90 days after ICU admission. The risk factors with significant differences were the patient’s severity based on the APACHE II score (P = .002), remain on IMV (P < .001), be a tracheostomy carrier (P = .009), the ICU stay (P = .002), and the team experienced in safety issues in charge of the IHT (P = .002). Those patients with PSI were transferred more often compared to those who didn’t (3.3 ± 2.8 vs 1.5 ± 1.1, respectively; P < .001).
Risk factors associated with the appearance of incidents related to patient safety during in-hospital transfers of critically ill patients at the ICU setting.
| IHT with PSI | IHT without PSI | P | |
|---|---|---|---|
| N = 112 (14%) | N = 693 (86%) | ||
| APACHE II (mean ± SD) | 21 ± 6.7 | 18.6 ± 7.4 | .002 |
| Age (mean ± SD) | 62.9 ± 12.2 | 62.5 ± 14.7 | .87 |
| Age | |||
| Age < 70 years | 76 (14.5%) | 447 (85.5%) | .52 |
| Age ≥ 70 years | 36 (12.8%) | 246 (87.2%) | |
| Sex | |||
| Woman | 25 (11.2%) | 199 (88.8%) | .161 |
| Man | 87 (15%) | 494 (85%) | |
| Shift | |||
| Morning | 94 (14.4%) | 559 (85.6%) | .65 |
| Afternoon | 13 (11.2%) | 103 (88.8%) | |
| Night | 5 (13.9%) | 31 (86.1%) | |
| Priority | |||
| Urgent | 54 (12.5%) | 378 (87.5%) | .22 |
| Scheduled | 58 (15.5%) | 315 (84.5%) | |
| Team | |||
| Safety experts | 49 (22.3%) | 171 (77.7%) | .002 |
| Other teams | 61 (10.9%) | 497 (89.1%) | |
| Reason for transfer | |||
| Diagnostic tests | 89 (14.4%) | 528 (85.6%) | .446 |
| Surgical room | 21 (13.4%) | 136 (86.6%) | |
| Other | 2 (6.5%) | 29 (93.5%) | |
| IMV | 75 (20.5%) | 291 (79.5%) | <.001 |
| Days on IMV (mean ± SD) | 23.2 ± 19.5 | 22 ± 23 | .6 |
| Mortality after 28 days | 7 (6.3%) | 57 (8.2%) | .56 |
| Mortality after 60 days | 16 (15%) | 97 (13.9%) | .77 |
| Mortality after 90 days | 19 (17%) | 112 (16.2%) | .83 |
| ICU stay [median (min; max)] | 26 (1; 105) | 17 (1; 136) | .002 |
| No. of transfers/patient | 3.3 ± 2.8 | 1.5 ± 1.05 | <.001 |
| Transfer within the first 48 h | 33 (11.7%) | 248 (88.3%) | .193 |
| Tracheostomy | 44 (19.2%) | 185 (80.8%) | .009 |
The multivariate analysis proved that the factors associated with IHT-related PSI were IMV, and the team experienced in patient safety issues [OR = 2.57 CI (1.60; 4.11), and 2.22 CI (1.44; 3.41), respectively (Table 4).
Multivariate risk factors associated with the appearance of incidents related to patient safety during in-hospital transfers of critically ill patients at the ICU setting.
| OR multivariate | P | ||
|---|---|---|---|
| Team | Other teams | 1 | <.001 |
| Safety experts | 2.257 (1.47; 3.48) | ||
| IMV | No | 1 | <.001 |
| Yes | 2.588 (1.61; 4.15) | ||
| Tracheostomy | No | 1 | .478 |
| Yes | 1.251 (0.67; 2.32) | ||
| APACHE II | 1.020 (0.99; 1.05) | 0.190 | |
| Days of ICU stay | 0.996 (0.99; 1.01) | 0.500 |
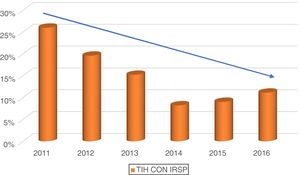
The biannual “IHT with PSI” indicator has evolved positively since the beginning of the registry while the “IHT with AE” indicator has remained < 5% (Fig. 2). After analyzing the evolution of the “IHT with PSI” indicator, the incidents were grouped into years while the study last quarter was discarded to eventually find statistical significance (P < .001) (Fig. 3). Considering the low number of AE found, the “IHT with AE” indicator shows no statistical significance.
DiscussionTo this date, there is not enough consensus in the medical literature available to establish quality standards that guarantee the safety of critically ill patients during IHTs. SEMICYUC21 recommends implementing a checklist that should include procedures and the equipment in 100% of the IHTs performed for diagnostic or therapeutic procedures. SEMICYUC also recommends that this checklist should be reviewed during the different stages of transfer. Regarding AE during IHTs, the “severe AE during IHT” indicator should be kept < 10%. Severe AE include death, recovered cardiac arrest, accidental extubation, catheter retrievals, access routes, drainages, and catheters, interruption of oxygen supply, and falls. In our study, in around 805 transfers, the “IHT with AE” indicator (any type of AE) was 2.4%, without any deaths, accidental extubations or falls.
The biannual monitoring of the “IHT with PSI” and “IHT with AE” safety indicators facilitate the identification of problems to be able to take actions of improvement. Like Beckmann8 we believe that monitoring incidents during IHTs should help improve the safety of critically ill patients on an ongoing basis.
On the other hand, implementing similar protocols in hospitals during the entire healthcare process, as well as during the management of critically ill patient to reduce PSI during IHT outside the ICU setting22 seems logical somehow.
In our study we found 112 IHTs where some PSI occurred (13.9%). In 93 transfers, a total of 136 HIs were notified, and in 19 HIs, AE were reported. The risk factors associated were the number of transfers per patient, severity based on the APACHE II score, IMV, be a tracheostomy carrier, and the team in charge of the transfer. IHTs with PSI were associated with longer ICU stays, but not with higher mortality rates. In the logistic regression analyses, only IMV and the team were significant factors.
Patients who underwent more transfers have more possibilities of sustaining PSI according to the different series published to this date, which is consistent with our study findings.23,24
A prospective and observational study considered IMV as a risk factor for IHT-related complications.14 Transfers have also been associated with a significant risk of invasive mechanical ventilation-associated pneumonia (MVAP).25,26 However, although in our series, IMV was the main risk factor for PSI, we didn’t find a higher rate of MVAP in a retrospective review of the 805 IHTs, just the same as in other series.7 The detection of PSI during the IHT was significantly associated with longer stays, but not with more days on IMV.
A French multicenter study described IHT-related AE in critically ill patients on IMV.9,27 A total of 3006 IHTs were performed to run diagnostic tests in 1782 patients on IMV. A total of 191 IHTs with incidents were found, 51 of which were severe (31%) with a 2% mortality rate. Incidents were associated with respiratory problems such as pneumothorax, atelectasis or MVAP, deep venous thrombosis, and metabolic problems. The IHTs made the hospital stay longer but did not increase the mortality rate.
In a recent study7 of 262 transfers of 184 patients on IMV, the rate of PSI was 45.8%, and the risk factors described were IMV with PEEP > 6 cm of H2O, sedation, and the fluids administered. In this study no increase of MVAP, time on IMV or ICU stay was reported.
The APACHE II score of IHTs where some PSI have been reported was not higher in the multivariate analysis unlike the Chinese series of 441 IHTs recently published.10 In this study, however, the rate of AE was 79.8%, far superior to ours. In other retrospective reviews, the rate of PSI was associated both with the patient’s severity and with IMV.23
Although tracheostomy was not statistically significant in the multivariate analysis, we believe this had to do with the greater statistical weight of IMV. The tracheostomized patients of our series have more PSI, longer stays, and require more transfers during their hospitalizations.
A total of 54.5% of the PSI reported had to do with the equipment, mainly the monitor and the ventilator, which is somehow similar to the rates disclosed by other studies.8,22,27–30 In the review conducted by Fanara et al.,13 22% of all AE were associated with problems with the ventilator.
The problems associated with the transfer team and the organization represented 30% and were associated with the lack of expert personnel according to the protocol, and with communication problems with the receiving hospital for lack of information passed on from one unit to the other at some point during the transfer.19
The disorders we found were basically hemodynamic in 47% of the cases and respiratory in 33% of the cases, same as in other series.6,27,28,31,32
We believe that in order to improve control during the transfer of patients with VAD and/or IMV, invasive arterial pressure monitorization should be implemented, as well as the capnography in compliance with the recommendations established by clinical practice guidelines.5,17,33
In our study the rate of protocol compliance was very high (> 90%) unlike other studies with protocol noncompliance rates > 27%, and higher rates of AE (18.18%).34
Although in other studies23,35 transfers within the first 48 hours were associated with more PSI, in our series, it was not a risk factor.
In 97.4% of all IHTs the transfer team including the treating doctor and the nurse assisting the patient. In a qualitative study recently published,36 86% of the transfers were performed by nurses and no doctors. Also, communication issues were found added to a lack of team work as possible risk factors. In a study already mentioned here, the team included resident and orderly. However, when the incident rate during the transfer of ventilated patients reached 45.8%, a nurse was added to the mix.7
IHTs should always be performed by a specialized team to reduce the rate of AE,5,6,16,28 especially if it is a senior team.8,15 We believe that our low rate of PSI during IHTs has to do with the experience of the medical and nursing teams involved, which is consistent with reports coming from other series.31,37 Also, with the addition of a second nurse to the transfers of more critically ill patients with IMV and VAD.
The number of incidents occurred during transfers performed by doctors who are safety experts is higher (49 out of the 112 IHTs, 44.5%) simply because the transfer more critically ill patients, have a greater safety culture and risk awareness, and notify more incidents compared to other doctors, but not the number of AE occurred. A recent retrospective study38 on the transfer of ventilated patients, with higher APACHE II scores, and performed by rapid response teams including intensivist plus trained nurse, did not find an impact in the occurrence of AE, which is suggestive that the patient’s severity, and not the experience of the transfer team, is actually associated with the occurrence of AE.
The likelihood of occurrence of PSI maybe directly proportional to the patient’s severity and to the amount of monitorization needed for the transfer. With the rise of extracorporeal membrane oxygenation (ECMO) techniques the rate of AE is much higher, and it seems necessary to increase our awareness on the importance of IHT in this very critically ill patients.39,40
We believe that the transfers of critically ill patients should be taken into consideration both in the training and the awareness surrounding the safety of patients.
The rate of PSI reported in our study was low compared to the medical literature available, which is possibly due to the fact that the procedure was performed following the existing recommendations7,13 like the meticulous preparation of the patient prior to his transfer, the patient/team dynamic assessment,8,17,27–29 the protocol follow-up,17,27 and the checklist run before the transfer.7,8,13,22 Finally, IHTs did not affect mortality, which is consistent with what other studies have reported on this regard.9,14
LimitationsAmong other limitations, we should mention the lack of external validity since this was not a multicenter study. The only setting studied was the in-hospital setting, which means that our conclusions may not be extrapolated to the complexity and technicity of out-of-hospital transfers that have become so popular these days.41 Also, in our unit we do not provide healthcare to neurocritical patients treated with ECMO or intra-aortic balloon counterpulsation (IABP) who are the ones who need more monitorization during the IHT.
On the other hand, the experience of the transfer ream is high, which explains the low number of PSI reported. Also, the changes made to the procedure across the study adding actions of improvement, as well as the experienced acquired since the implementation of the protocol may have impacted the results reported.
ConclusionsThe number of IHT-related PSI in critically ill patients at the ICU setting after the implementation and follow-up of a protocol is low compared to the medical literature available, being IMV the main risk factor. The safety expert team declares a higher number of incidents, and also transfers the most critically ill patients The biannual evolution of safety indicators associated with the transfers is significantly favorable allowing us to establish our own standard.
Authors/collaboratorsRMCI, MCMD, and NRC designed the study. RMCI, EZC, MLA, JLLC, JPGV, MCS, and MJC contributed to collecting data from the transfers. EPJ performed the statistical analysis.
All the authors made important intellectual contributions to the study, and participated actively in the interpretation of data, and in the writing of the manuscript. All the authors contributed to the manuscript critical review and approved its final version.
FundingDr. R.M. Catalán received a Bayés scholarship - FORES (Fundació d’Osona per a la Recerca i l’Educació Sanitària”).
Conflicts of interestNone reported.
We wish to thank the medical and nursing team at the Hospital Universitario de Vic Intensive Care Unit for their dedication and help writing down the protocol. Also, for collecting data from all in-hospital transfers performed and included in this study. Also, we wish to thank the multidisciplinary team, so involved in this project, for improving safety measures at the ICU setting. Finally, we wish to thank the Epidemiology Unit personnel for their unvaluable help and support.
Please cite this article as: Catalán-Ibars RM, Martín-Delgado MC, Puigoriol-Juvanteny E, Zapater-Casanova E, Lopez-Alabern M, Lopera-Caballero JL, et al. Incidentes relacionados con la seguridad del paciente crítico durante los traslados intrahospitalarios. Med Intensiva. 2022;46:14–22.