Edited by: Alberto García-Salido - Pediatric Intensive Care Unit, Hospital Infantil Universitario Niño Jesús, Madrid, Spain
Last update: May 2024
More infoAcute confusional state or delirium is one of the most common complications associated with stays at the intensive care unit (ICU) setting. This disorder affects over half of the critically ill patients admitted to these units, which increases the length of stay (LoS), the annual hospital costs, and is independently associated with a higher mortality risk.1
The main challenges associated with this disorder are its prevention, and early detection, and management. Different medical associations like the Society of Critical Care Medicine and the Spanish Society of Intensive and Critical Care Medicine and Coronary Units claim that especially after the COVID-19 pandemic, the early identification of this disorder in critically ill patients is of paramount importance.2 Also, they discuss measures like the ABCDEF algorithm as the cornerstone of the pharmacological management of delirium.1 Despite showing some implementation difficulties, these measures have proven capable of reducing the duration of delirium and the patients’ LoS. This was initially exposed in the studies conducted by Ely and Marra et al.3,4 that discussed the measures that could improve the management of critically ill patients. Among these measures—particularly letter «D» from the ABCDEF algorithm—the authors stress out the importance of assessment, prevention, and management of delirium in adult patients.
The same tendency has arrived at the pediatric setting where specific guides and protocols are scarce, especially in our country. Over the past decade, different scales have been developed and validated for the detection of delirium in the pediatric patient such as the Pediatric Confusion Assessment Method for the Intensive Care Unit or the Sophia Observation withdrawal Symptoms scale, and among them, the Cornell Assessment of Pediatric Delirium (Table 1).5 Despite of this, different trials conducted recently show how difficult it is for healthcare professionals to identify this disorder—misdiagnosed in up to 71% of the cases—since routine screening is conducted in 2% of the cases only.6
Cornell assessment of pediatric delirium.
| If RASS score −4 or −5 (deep sedations/does not wake up) CAPD won’t be necessary | ||||
| 1. Does the child make contact with the caregiver? | ||||
| 2. Are the child’s actions purposeful? | ||||
| 3. Is the child aware of his/her surroundings? | ||||
| 4. Does the child communicate needs and wants? | ||||
| 4 (Never) | 3 (Rarely) | 2 (Occasionally) | 1 (Often) | 0 (Always) |
| 5. Is the child restless? | ||||
| 6. Is the child inconsolable? | ||||
| 7. Is the child underactive—very little movement while awake? | ||||
| 8. Does it take the child a long time to respond to interactions? | ||||
| 0 (Never) | 1 (Rarely) | 2 (Occasionally) | 3 (Often) | 4 (Always) |
| Presence of delirium if overall score ≥ 9 | ||||
The studies and surveys conducted so far show the need to train pediatric intensive care units (PICU) personnel on the management of delirium, especially in the identification and control of the risk factors that can eventually trigger it.6,7 Similarly, they focus on a certain paradigm shift and greater safety perception from the PICU staff after being trained on the management of delirium and, especially, after the adoption of guidelines on the multidisciplinary management of this entity. The use of these guidelines improves communication among the different health professionals involved and, implicitly, the management of pain and sedation in children.8
Following this multidisciplinary line of work and in compliance with the evidence reviewed, the prevention and management of this disorder in children is based on controlling the modifiable risk factors involved which, added to the patient’s underlying disease, can trigger delirium. These risk factors include pharmacological and non-pharmacological elements, so they need the participation of different health professionals for a holistic approach of these patients. Therefore, the evidence available to this date confirms the need to include measures aimed not only at preventing and assessing delirium, but also at detecting its possible causes. The use of different acronyms helps here like those collected by different working groups like I WATCH DEATH or BRAIN MAPS that reveal some of the causes that can lead to the appearance of this disorder.9,10 At this point, a distinction should be made regarding symptom overlap between delirium and abstinence syndrome or pharmacological withdrawal. In this case, more than a limitation for the early detection of delirium, deprivation syndrome can be among the causes of acute confusional state, which is why some authors say that the goal here is to determine and treat the cause of delirium rather than somehow «segment» its approach.11 On the other hand, there is no doubt that sedation and analgesia protocols are of paramount importance to reduce the use of benzodiazepines and overdosing in children. However, a universal sedation protocol has not been established yet. As a matter of fact, this is one of the main challenges posed by the management of delirium in children.
Over the last few years, different working groups have conducted pre- and postoperative studies to determine the room for improvement associated with the use of measures to assess and control this disorder, and the possible difficulties involved while trying to implement them. These studies have been promising reducing the prevalence of delirium—especially in children under 5—and increasing compliance regarding the screening of delirium by healthcare professionals.9,12 Although there are different variables like the LoS at the ICU setting, results have been inconclusive.10
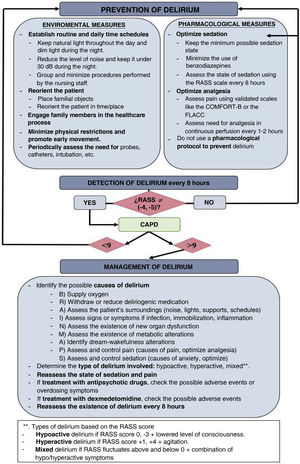
One of the most common complaints made by the health professionals after implementing these measures is how difficult it is to balance the management of patients and the observance of scales and delirium prevention measures due to working load constraints and the limited amount of time available for each patient. Another aspect that seems to prevent the proper development of screening is the fact that the hours selected for this purpose are not the most suitable ones since they coincide with the heaviest working loads during the shifts.13 Simplifying these measures or adding them to easy-to-read algorithms would favor the implementation and observance of these measures by the health professionals. In this context, one of the scales that seems to reduce the time of screening because of how easy it is to use, and because it has shown a high correlation and reliability compared to other scales that study sedation in critically ill children is the Richmond Agitation Sedation Scale14 (Table 2). On this regard, the use of the algorithm included in Fig. 1 is suggested. This algorithm includes measures aimed at prevention, early detection, and management of delirium based on a review of the current evidence available.
Richmond agitation sedation scale.
| 4 | Combative | Overtly combative, violent, immediate danger to staff |
| 3 | Very agitated | Pulls or removes tube(s) or catheter(s); aggressive |
| 2 | Agitated | Frequent non-purposeful movement, fights ventilator |
| 1 | Restless | Anxious but movements not aggressive vigorous |
| 0 | Alert and calm | |
| −1 | Drowsy | Not fully alert but has sustained awakening. Eye-opening/eye contact +10 s |
| −2 | Light sedation | Briefly awakens with eye contact to voice. Eye-opening/eye contact −10 s |
| −3 | Moderate sedation | Movement or eye opening to voice (but no eye contact). |
| −4 | Deep sedation | Unresponsive to voice, but movement or eye opening to physical stimulation |
| −5 | Unarousable | Unresponsive to voice or physical stimulation |
There is no question that raising awareness on the importance of all that surrounds the critically ill patient improves this culture of care at the ICU setting in our country. However, more effort and dedication are needed to develop and implement protocols and measures to ease the management of pediatric critically ill patients. Another possible line of work here could be to detect the difficulties we face and recognize the areas of knowledge where those in charge of these patients still find barriers or limitations. Training, motivation, and the involvement of different health professionals are essential to improve care and bring pharmacological and non-pharmacological strategies to terms regarding the management of pediatric delirium.
Conflicts of interestNone whatsoever.