Sepsis is a syndromic entity with high prevalence and mortality. The management of sepsis is standardized and exhibits time-dependent efficiency. However, the management of patients with sepsis is complex. The heterogeneity of the forms of presentation can make it difficult to detect and manage such cases, in the same way as differences in training, professional competences or the availability of health resources. The Advisory Commission for Patient Care with Sepsis (CAAPAS), comprising 7 scientific societies, the Emergency Medical System (SEM) and the Catalan Health Service (CatSalut), have developed the Interhospital Sepsis Code (CSI) in Catalonia (Spain). The general objective of the CSI is to increase awareness, promote early detection and facilitate initial care and interhospital coordination to attend septic patients in a homogeneous manner throughout Catalonia.
La sepsis es una entidad sindrómica de elevada prevalencia y mortalidad. Su manejo está estandarizado y tiene una eficacia dependiente del tiempo. Sin embargo, el manejo de los pacientes con sepsis es complejo. La heterogeneidad de las formas de presentación puede dificultar su detección y manejo, así como las diferencias en formación, competencias o disponibilidad de recursos sanitarios. La Comisión Asesora para la Atención al PAciente con Sepsis (CAAPAS), formada por 7 sociedades científicas, el Sistema de Emergencias Médicas y el Servei Català de la Salut, han desarrollado en Catalunya el Código Sepsis Interhospitalario (CSI). El objetivo general del CSI es facilitar la detección precoz, la atención inicial y la coordinación interhospitalaria para optimizar el tratamiento de los pacientes con sepsis o shock séptico en formato código de riesgo vital, de forma homogénea a lo largo de todo el territorio catalán.
Sepsis is a syndrome induced by an infectious process that leads to the dysregulation of inflammatory response causing acute or exacerbated organ dysfunction. Sepsis presenting with hypotension that does not respond to volume restoration, lactacidemia or requires vasoactive drugs to keep tissue perfusion is called septic shock. Its detection is based on physical examination and the assessment of the infection systemic repercussion. Its severity can be stratified according to the number and/or degree of organs damaged. The SOFA score is recommended as a descriptive element of the degree of severity.1
The incidence of sepsis increases gradually in industrialized countries in between 200 and 400 cases per 100 000 people/year.2–4 The cost associated with the management of severe sepsis depends on several factors and increases exponentially with the magnitude of organ failure.5 Its mortality rate is around 20%–30% and is affected by non-modifiable (characteristics of the patient, focus of infection, culprit microorganism) and modifiable factors. The most significant ones are time to restore tissue perfusion, and adequacy in the management of the septic focus (time to antibiotic treatment, adequacy of empirical coverage, and drainage of the septic focus, if necessary).6–8
However, the existence of protocols to optimize the management of any conditions is a necessary yet insufficient requirement.9 When dealing with complex or difficult to diagnose conditions or having to coordinate different healthcare resources, implementation strategies need to be designed to favor their use in the routine clinical practice. Given the high incidence and morbimortality associated with sepsis and the existence of standard guidelines on the diagnosis and management of sepsis,10 and the correlation between early treatment and functional and vital prognosis11–16, we should agree that the management of sepsis should meet certain «critical code» criteria. Also, in the management of septic patients, the necessary human resources, skills, and technology for the diagnosis, management of the septic focus and advanced support (especially hemodynamic, mechanical ventilation, and hemofiltration) in cases of organ failure may not be available in all centers assisting acute patients. That is why coordination among the different levels of healthcare is essential at this point. Also, the need to maintain a time-dependent concept in the management of multi-organ failure in patients with sepsis requires the implementation of strategies for interhospital coordination.
Sepsis in Catalonia. Advisory commission on the management of patients with sepsis (CAAPAS). Goals of code sepsisSeven point five million people live in Catalonia, Spain where sepsis affected 80 000 patients between 2008 and 2012 with an average of over 16 000 patients/year, showing a continuous annual increase.5 Up to 25% of these patients may end up requiring healthcare in Intensive Care Units (ICU). According to a population-based prospective study conducted by Almirall et al. community-acquired sepsis causes 47 ICU admissions per 100 000 patients/year. Regarding hospital stays, it leads to the occupation of 2 beds/day/100 000 people.17
The Catalan healthcare model has some differences compared to other models in Spain. One of these differences is that an important number of hospital beds are found in regional hospitals that have a high volume of ER cases and, therefore, a great capacity to detect cases. However, not all hospitals have the human or technological resources required to manage the most severe or evolved cases of sepsis. Forty per cent of all Catalan hospitals do not have ICUs available to assist adult patients and there are only 5 pediatric ICUs in the entire Catalan territory.
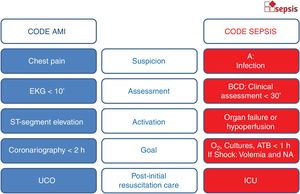
During the first decade of the 21st century, the Catalan Health Service (CatSalut) implemented 3 critical codes: infarction code, polytrauma code, and stroke code. In the management of sepsis, different hospitals and research groups have been working on healthcare circuits and training resources in Catalonia to improve the management of patients with severe sepsis.18–20 These initiatives presented by the Catalan Society of Intensive and Critical Care Medicine (SOCMIC) started contacts for the implementation of the «Interhospital Code Sepsis» within the existing critical codes (Fig. 1) to provide homogeneous coverage to all patients in the healthcare system regardless of where the first care takes place. The SOCMIC Sepsis Working Group was created back in 2012 and evolved into the Advisory Commission on the Management of Patients with Sepsis (CAAPAS) in 2014. This Commission included 7 scientific societies representative of the Catalan intensive care setting: SOCMIC, Emergencies (Catalan Society of Urgent and Emergent Care Medicine [SOCMUE]), Internal Medicine (Catalan-Balearic Society of Internal Medicine [SCMI]), Surgery (Catalan Society of Surgery), Infectious (Catalan Society of Infectious Diseases and Clinical Microbiology [SCMIiMC]), Family Medicine (Catalan Society of Family and Community Medicine [CAMFIC]), and Pediatrics (Catalan Society of Pediatrics). These societies were backed by their corresponding boards of directors with help from the Emergency Medical Service (EMS) that manages emergent out-of-hospital care and the interhospital transfers of critically ill patients, and with representation from the Catalan Health Service (CatSalut).
Aware of the social upheaval created by sepsis, the Parliament of Catalonia passed Resolution 1069/X back in June 19th, 2015 recognizing sepsis as a life-threatening entity. It also urged the Government of Catalonia to actually «define and coordinate all the necessary measures to implement the Code Severe Sepsis in 2015 as a brand new code of medical emergencies».21 The recommendations given by the CAAPAS have been taken over by the CatSalut to structure CODE SEPSIS («Codi Sèpsia» in Catalan) published as an operative instruction for all hospitals in the Catalan public health system (Instruction 11/2015 of October 8th, 2015).22
Goals of Catalonia’s «Code Sepsis»In the setting of patients with infectious processes, there are 3 different clinical scenarios that make up a different healthcare context: «infection», «sepsis», and «septic shock». The recent review of the definition of sepsis recommends the objective assessment of the degree of multi-organ dysfunction using the SOFA score.23 Also, its use is recommended as a descriptive element of systemic repercussion. We define «sepsis» as a subgroup of infections causing at least acute (SOFA ≥ 2) or exacerbated organ failure (baseline SOFA increase ≥ 2). We define «septic shock» as an infection that yet despite proper resuscitation with serum still requires vasoactive drugs to revert a situation of tissue hypoperfusion, hypotension or lactacidemia. Multi-organ failure is defined as a clinical scenario of, at least, 2 SOFA categories scoring >2.
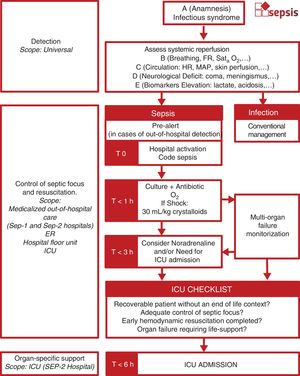
The general goal of Code Sepsis (CS) is to facilitate early detection, initial care, and interhospital coordination to optimize the management of patients with sepsis or septic shock in the format of a life-threatening situation. CS proposes a time-dependent staged procedure with interhospital coordination for septic patients (Table 1).
Differences among different scoring systems proposed for the assessment of systemic repercussion after infections in the adult patient.
| Code Sepsis | qSOFA28 | NEWS30 | SIRS29 | |
|---|---|---|---|---|
| A: Anamnesis | Infectious syndrome | |||
| B: Breathing | Tachypnea (suspicion) | Tachypnea | Tachypnea | Tachypnea |
| Hypoxia (activation) | Hypoxia | |||
| Oxygen therapy | ||||
| C: Circulation | Tachycardia (suspicion) | Tachycardia | Tachycardia | |
| Hypotension (activation) | Hypotension | Hypotension | ||
| D: Dissability/Neurological | Altered level of consciousness (suspicion) | Altered level of consciousness | Altered level of consciousness | |
| Meningismus(activation) | ||||
| E: High biomarkers | Lactate | Leukocytosis | ||
| Other | Temperature | Temperature |
These are its specific goals:
- -
Raise awareness and train the healthcare personnel in the importance of early detection and management of severe sepsis.
- -
Agree on the criteria to be met for the early detection and management of patients with severe sepsis.
- -
Standardize early management (resuscitation) by identifying severity criteria and poor patient progression.
- -
Assess all the necessary criteria and circuits structuring interhospital coordination to enter the patient in the right level of healthcare.
- -
Follow-up, analyze, and provide feedback of the epidemiological indicators of activity, process, and outcomes.
We can identify 4 different stages in the management of sepsis following the detection of a septic patient:
- -
Activation.
- -
Control of the focus of infection and hemodynamic recovery.
- -
Organ-specific support. Referral to the ICU.
- -
Resolution of sepsis.
To facilitate the early identification of signs suggestive of organ dysfunction by the healthcare personnel in patients with a past clinical history of infection. It requires minimal technological support and can be initiated anywhere, whether at the hospital or the out-of-hospital setting.
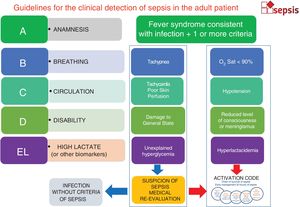
Systemic repercussion should be clinically assessed in all patients with an infectious process. Given the actual debate on how to optimize the assessment of the presence or risk of sepsis in an infection,24–27 the need for ICU admission or mortality risk, and to be respectful with each center, the CAAPAS proposed the systemic repercussion of infections. The proposed format was A + BCD + E (for the assessment of both adult and pediatric patients) and it is consistent with the clinical assessment made by the SOFA, qSOFA,28 SIRS29 or EWS scores30 (Fig. 1). The diagnosis of sepsis should be predominantly clinical. We shouldn’t wait for the results of the blood test to activate the CS because we could be delaying maneuvers unnecessarily. The proposal is to assess whether there is risk of systemic repercussion in every patient with anamnesis consistent with a clinical infection at the beginning and then use risk biomarkers only if necessary.
Here is the proposal (Fig. 2):
Algorithm for the detection of the adult septic patient. Clinical detection based on cardiovascular, respiratory, and neurological assessment. Tachycardia and Tachypnea are considered adaptative responses that may anticipate the appearance of organ failure. Numerical values have been eliminated as much as possible because there is no consensus on which the cut-off values are in the different scoring systems that different centers may be using. In the presence of organ failure, it allows the activation of code sepsis. In cases of out-of-hospital detection, it is advisable to pre-alert those involved in the screening stage at the gates of the ER (sepsis pre-alert).
A. Anamnesis: Clinical history and/or physical examination indicative of an infection.
B. Breathing: assess respiratory distress.
C. Circulation: assess circulatory dysfunction.
D. Dissability/Neurological focality: assess meningismus or altered level of consciousness
E. Biochemical assessment: lactate/other biomarkers of tissue hypoperfusion or organ failure (at the hospital setting).
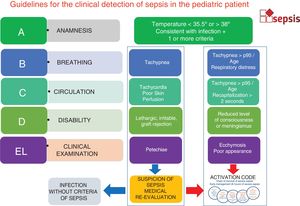
The pediatric patient has some particularities like signs of a poor general state, the appearance of petechiae or poor skin perfusion (Fig. 3).
Algorithm for the detection of the pediatric septic patient. Clinical detection based on cardiovascular, respiratory, and neurological assessment. In the presence of organ failure, it allows the activation of code sepsis. In cases of out-of-hospital detection, it is advisable to pre-alert those involved in the screening stage at the gates of the ER (sepsis pre-alert).
The CS should be activated in a patient with sepsis or septic shock (anamnesis consistent with infectious syndrome plus organ failure [B, C or D] and/or early hyperlactacidemia), treated at the hospital setting, who is not at the end of his life, and without any limitations to use life support techniques. The management of sepsis and the decision to assist in code format should be spared for patients with anticipated last wills contrary to receiving treatment against the focus of infection or life support measures. These procedures are very common in the management of septic patients, patients with severe cognitive impairment or terminally ill patients without detriment to the basic measures used in all patients (oxygen therapy, volemia restoration, administration of antibiotics, etc.).
Although the administrative activation of the code happens at the hospital, there is an out-of-hospital sepsis pre-alert that is activated by Primary Care Teams, out-of-hospital urgent and/or continuous care devices, EMS Basic, Intermediate or Advanced Care Units, etc. that assist patients with infections and meet the agreed criteria. Resuscitation maneuvers will be initiated when appropriate. In this case, the EMS will be transferring patients eligible for CS activation with severity-adjusted priority to nearby hospitals capable of confirming clinical diagnosis, CS activation, lab diagnosis, and actions performed at the resuscitation phase (control of the focus of the infection, administration of volume, monitorization, etc.). The EMS will be transferring patients to centers with higher levels of healthcare when the patient’s clinical progression suggests immediate ICU care and following the criteria established for life-threatening cases.
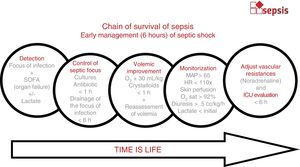
Stage 2. Control of the focus of infection and hemodynamic recoveryThe control of the focus of infection is based on a package of 5 steps (Fig. 4):
- -
Patient already identified as eligible to be treated in code format.
- -
Early administration of empirical antibiotics effective enough to reduce bacterial load (together with drainage of the focus of infection, if necessary).
- -
The restoration of oxygen tissue perfusion through volemia restoration and oxygen therapy.
- -
The monitorization of the patient’s response to early measures.
- -
The clinical and analytical assessment of organ failure and the need for a higher level of critical care (ICU).
Steps for the management of sepsis. Package of actions to be implemented after the detection of patients with sepsis: immediate administration of oxygen, hemocultures, blood tests, and administration of antibiotics. If signs of hypoperfusion, administer 30 mL of crystalloids per kg of weight in 1 h and monitor volemic status if unresponsive. Consider the administration of noradrenaline in patients with signs of deep hypoperfusion or who remain unresponsive to early volume loads. Consider ICU referral if unresponsive to early maneuvers.
The basic component of CS is the identification of the case, the administration of empirical antibiotic therapy, and the initiation of maneuvers to restore tissue perfusion. For this reason, centers should have a protocol available for the management of specific empirical antibiotic therapy for CS, validated by the commission of infections of the corresponding center, and a protocol on hemodynamic management consistent with the resources and capabilities of each particular center and based on the updated recommendations provided by the Surviving Sepsis Campaign. The admission of patients to the ICU (from the referring center where the patient is hospitalized) is just another part of the healthcare process that implies the failure of resuscitation maneuvers or severity conditioning the use of life support techniques.
Resuscitation and the control of the focus of infection should be adapted to the patient’s clinical status. Septic shocks should be considered a life-threatening situation. The goals within the first hours of care are to restore the correct oxygen tissue perfusion, complete the syndromic diagnosis, draw blood samples for culture purposes, and administer early empirical antibiotic therapy preferably within the first hour of care.31 Placing central venous catheters or conducting the corresponding imaging modalities should not delay resuscitation maneuvers or the control of the focus of infection.32 We recommend the clinical (cardiovascular, respiratory, and neurological) and analytical monitoring of the septic patient with controls within the first 6 h. The analytic control of lactate is mandatory when the early test is pathological.
Although the optimal venous access for the administration of vasoactive drugs is the lumen of a central IV used only for this purpose as it is the case with patients with shock, it is not advisable to delay the initiation of noradrenaline until obtaining a central IV because the process can delay hemodynamic recovery significantly. In this case, we suggest using a single peripheral catheter inserted in a vein of the largest caliber possible of the upper limb where arterial pressure is not being monitored non-invasively while limiting the mobility of the arm as much as possible. Once noradrenaline has been initiated, it is advisable not to keep it via peripheral route for more than 6 h because it increases the risk of complications.33,34
If the control of the focus of infection requires surgical management, it should be performed within the first 6 h when the patient is in septic shock. In septic patients without shock, the surgical decision should be individualized but not be delayed for more than 12 h.
In cases of partial response or organ failure persistence despite an adequate early resuscitation, if the patient requires more monitorization and/or the use of specific diagnostic and therapeutic tools by trained professionals (nurses and doctors) for the management of different organ failures and/or the implementation of organ-specific support techniques (vasoactive drugs, mechanical ventilation, renal replacement therapy), the reference ICU should be informed to anticipate possible hospitalizations. This unit should be accredited to provide continuous multidisciplinary care to critically ill patients in a specific setting with enough functional, structural, and organizational means for admission purposes.
Stage 3. Organ-specific support. Referral to the ICUIn Catalonia, unlike the acute myocardial infarction code and like the stroke code, patients are not eligible for direct transfer to the ICU, but it is the reference intensivist who makes this decision through the EMS (Fig. 5). The transfer of patients to centers with higher levels of healthcare and ICU should be coordinated through the EMS Central Headquarters in order to transfer each patient to the hospital with the most suitable level of healthcare. To optimize the management of these patients, it is necessary to share the necessary information between the doctor in charge of the referring center and the intensivist of reference of the receiving center including focus of infection, systemic repercussion, lack of life-sustaining treatment limitation, right resuscitation maneuvers, degree of multi-organ failure, need for organ-specific support required, etc., and eventually agree on future actions. If indicated, the transfer of patients should happen on a Life Support Unit with patient-adjusted priority level, up to 3 h for sepsis (organ failure without hemodynamic instability), and priority 0 in the case of septic shock or multi-organ failure.
Algorithm for interhospital coordination. Out-of-hospital pre-alerts notify the ER screening system so they can anticipate the emergent management of patients under code sepsis. Checklist requires 4 of out 4 affirmative answers to agree on the transfer of patients between referring and receiving hospitals.
Once resuscitation maneuvers have started and the focus of the infection is under control, different criteria should be considered when assessing referrals to the UCI:
- 1
Lack of clinical improvement within the first 3–6 hours after initiating the resuscitation measures in adult patients.
- 2
Need for more complex organ-specific support (invasive mechanical ventilation, management of hemodynamic instability, vasoactive support and advanced cardiovascular monitorization, renal clearance techniques, ECMO, etc.).
- 3
Similarly, referral to more complex centers, lack of resources for the correct diagnosis or drainage of the focus of infection (percutaneous drainage, complex surgeries, etc.) should all be taken into consideration without detriment to the initiation of hemodynamic resuscitation maneuvers.
The resolution of the event includes referring the patient to the corresponding hospital—preferably the referring center—depending on the therapeutic requirements.
Interhospital coordination. Levels of healthcare and flow of patientsThe right care should be provided within the level of healthcare that best suits the needs of each patient, at the right time, and based on the severity of the patient’s clinical status. Categorizing the territory into coordinated hospital clusters facilitates the creation of working groups and the arrangement of the right flows by matching the criteria of severity of each patient to the right level of healthcare required (Table 2).
Example of hospital distribution: hospital cluster in the Barcelonès Nord/Maresme area in the adult patient.
| Area | Level | Reference SEP-2a center | Reference SEP-2b center |
|---|---|---|---|
| Hospital de Calella | SEP-1 | Hospital de Mataró | H. Germans Trias i Pujol |
| Hospital Esperit Sant | SEP-1 | H. Germans Trias i Pujol | H. Germans Trias i Pujol |
| Hospital Municipal de Badalona | SEP-1 | H. Germans Trias i Pujol | H. Germans Trias i Pujol |
| Hospital de Mataró | SEP-2a | Hospital de Mataró | H. Germans Trias i Pujol |
| Hospital Germans Trias i Pujol | SEP-2b | H. Germans Trias i Pujol | H. Germans Trias i Pujol |
SEP-1: hospitals capable of implementing the stages of detection, activation, and resuscitation-control of the focus of infection; SEP-2; hospitals capable of implementing the stages of organ-specific support (have ICUs available) but without 24/7 logistics regarding the surgical management of certain septic foci. SEP-2b: SEP-2 (ICU) hospitals powered to perform the surgical management of all septic foci on a 24/7 basis. Every level includes the previous one.
Acute care hospitals for the management of adult patients are categorized into 3 levels depending on their functional capabilities:
- -
Hospitals with resources available for the stage of resuscitation and control of the focus of the infection are classified as SEP-1 centers.
- -
Hospitals with ICU capabilities (specific-organ support) classified as SEP-2 centers.
- -
SEP-2 centers are considered SEP-2b when they are reference centers capable of controlling de focus of the infection under special conditions and performing the surgical control of septic foci different from abdominal and soft-tissue foci on a 24/7 basis (control of the obstructive urinary focus, control of thoracic focus, neurosurgical, etc.).
- -
A SEP-2b reference center is assigned to all SEP-1 and SEP-2 centers where patients can be referred to when necessary.
- -
All hospitals include their lower level of healthcare.
The pediatric model is similar with some particularities. Acute care hospitals for pediatric patients are also categorized into 3 levels:
- -
Hospitals capable of managing the stage of resuscitation and controlling the focus of the infection are classified as SEP-1 centers.
- -
Hospitals with pediatric ICU capabilities are classified as SEP-2a.
- -
SEP-2 hospitals are classified as 2b only if they can provide ECMO support.
- -
All hospitals include their lower level of healthcare.
The goal of the registry is to consider actions that may facilitate making proposals for improvement for every center and the overall healthcare system to reach the goals of the project in the implementation of CS. Two parallel registries are suggested on this regard:
- -
Automatized Registry of Administrative Data Regarding Sepsis (RADAR-Sepsis): based on data obtained from coding hospital discharges and comorbidity data provided by CatSalut. Its goal is to generate a panel for the comparative analysis of epidemiology, results, and use of associated resources. It allows getting feedback from the events provided by different health areas and hospitals.5,34–37
- -
Registre de Sèpsia i Xoc Sèptic (RSiXS): prospective registry hosted at the «Applications Portal» and owned by the Department of Health of the Government of Catalonia since October 2018.33 It prospectively collects epidemiological indicators. Also, event, process, use, and result indicators to analyze avoidable mortality in septic patients requiring ICU admission. The indicators recommended by SEMICYUC,38 are considered key process indicators, although adapted to the new recommendations:32
- ◦
Early initiation of antibiotic therapy in patients with sepsis and/or septic shock within the first hour.
- ◦
The right empirical antibiotic therapy.
- ◦
Early resuscitation of septic shock within the first hour following detection:
- •
Restoration of 30 mL/kg of weight.
- •
- ◦
- •
Administration of noradrenaline if hypotension is refractory to volemia.
- •
Detection time of mean arterial pressure >65 mmHg.
The «Interhospital Code Sepsis» (ICS) proposes a new territorial organizational model to respect the harmony of every center when they activate their own code sepsis and provide territorial organization to facilitate the flow of patients and agreed methodologies and criteria for more agile coordination among the different healthcare providers involved.
FundingThis project has been partially funded by TV3 Fundació Marató (Sepsis Training, Audit and Feedback (STAF) Project; Codi Projecte 201836).
Conflicts of interestAll authors declared no conflicts of interest while conducting this project.
We wish to thank Ms. Emma Bosch for developing and supplying the logos for «Code Sepsis».
Please cite this article as: Yébenes JC, Lorencio C, Esteban E, Espinosa L, Badia JM, Capdevila JA, et al. Código Sepsis Interhospitalario en Catalunya: modelo organizativo territorial para la atención inicial al paciente con sepsis. Med Intensiva. 2020;44:36–45.