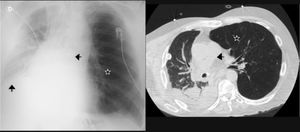
A 59-year-old patient with chronic obstructive pulmonary disease (emphysema) operated upon in childhood due to coarctation of the aorta, with aortic valve replacement surgery due to severe stenosis (anticoagulated with acenocoumarol), reported for two-lung transplantation. Because of the high surgical risk, single lung transplantation was decided, and anticoagulation with sodium heparin was started after 24h. On day 7 post-transplantation the patient suffered sudden dyspnea, tachycardia, paleness and fresh blood output from the pleural drain. Urgent revision surgery was decided, with the evacuation of a 300-ml hematoma. The bleeding point was not identified. The situation was complicated by hyperinsufflation of the native lung (Fig. 1, star) and right phrenic nerve paralysis (ascending arrow), giving rise to mediastinal displacement (arrow to left). Following surgical cleansing and physiotherapy, the clinical course proved favorable and discharge was decided.
Please cite this article as: Arlabán Carpintero M, Sánchez Arguiano J, Ballesteros Sanz MA. Hematoma intrapleural e hiperinsuflación del pulmón nativo en paciente con trasplante pulmonar. Med Intensiva. 2019;43:326.