The present letter describes the results of a study on the subjectiveness and analysis of different points of view regarding the ethical aspects and costs of treatments at end of life as perceived by the staff of an Intensive Care Unit (ICU), based on Q methodology.
In studies based on Q methodology, the interviewee – through a statement classification procedure known as the “q-set” – offers his or her point of view about a given study topic. Person factors analysis is subsequently used to identify significant correlation groups that can be interpreted as distinguishable points of view.1–7
The Q methodological approach to data analysis implies the sequential utilization of three statistical procedures: correlation, factor analysis and factor computing.8
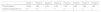
A total of 44 interviews were carried out. The first factor analysis applied to the correlation matrix identified 8 factors. The value corresponding to each factor, and the explained percentage of variance, are reported in Table 1.
The scree plot of the factors obtained showed a flattening of the curve to the right of the third factor. We therefore selected the first three factors for the posterior rotational (varimax) analysis.
The correlation between factor 1 and factor 2 was 0.41; that between factor 1 and factor 3 was 0.46; and that between factor 2 and factor 3 was 0.58.
Table 2 presents the full composition of the statements for the three factors, showing the ideal positioning of the statements in the grid, for each of the points of view.
Full composition of the statements referred to the three factors (Z-score).
| No. | Statement | Factor 1 | Factor 2 | Factor 3 | Z-score variance |
|---|---|---|---|---|---|
| 1 | Patients must have the right to reject life-prolonging treatments if they so wish | 2 | 2 | 3 | 0.086 |
| 2 | At the end of life, patients should be cared for at home with the best quality of life, instead of receiving aggressive and costly treatments that only prolong life for a short period of time | 2 | 2 | 2 | 0.098 |
| 3 | If a patient wishes to continue the struggle for as long as possible, this should be allowed, regardless of the cost | 1 | −2 | −1 | 0.577 |
| 4 | It is necessary to grant the patient and family the time need for preparing to die, put personal affairs in order, and make up and say goodbye to whoever the patient wishes | 3 | 1 | 1 | 0.245 |
| 5 | More value would be placed on treatments at end of life than many medical treatments for non-terminal disorders | −1 | −2 | 0 | 0.118 |
| 6 | High-cost drugs that are administered to terminal patients but offer few benefits, could be regarded as undue use of public funds | 0 | 2 | 1 | 0.206 |
| 7 | It is human nature to want to preserve life and continue living for as long as possible. It is one of our most basic instincts | 1 | 0 | 2 | 0.224 |
| 8 | If there is only one possibility of treatment, at a high cost, for prolonging the life of terminal patients, it should be made available | 0 | −2 | 0 | 0.422 |
| 9 | It might not seem like much, but a few additional weeks or months can be very important for a family with a terminally ill relative | 3 | 0 | 1 | 0.544 |
| 10 | Life should only be prolonged if the quality of life of the patient during that time will be good | 1 | 2 | −1 | 0.542 |
| 11 | It is preferable to allow death with dignity through compassion and selfless help than to administer drugs that grant a few more weeks or months of life for a very ill individual | 0 | 3 | 3 | 0.632 |
| 12 | One year of life has the same value for everyone | −3 | −1 | −2 | 0.122 |
| 13 | Funding should be allotted proportionally to those patients which we feel have not fairly received a possibility in terms of quality or duration of life | 0 | −1 | 1 | 0.247 |
| 14 | From a moral perspective, it is correct and beneficial to prolong the life of a terminally ill patient | −1 | −2 | −3 | 0.308 |
| 15 | If there are means for helping someone to live longer, it is morally incorrect to deny him or her those means | 1 | −1 | 0 | 0.249 |
| 16 | Failing to provide a terminal patient with access to drugs that can prolong life is equivalent to killing that patient | −3 | −3 | −2 | 0.099 |
| 17 | Treatments that are of high cost in relation to the health benefits they offer should be discarded | −2 | 0 | −2 | 0.299 |
| 18 | End of life medications are not a cure – they only prolong life. It makes no sense to delay the unavoidable for only a short time | −2 | 1 | −1 | 0.564 |
| 19 | Terminal patients may hold hope, but that is not a valid argument for providing costly treatments that can only prolong life for a short period of time | −1 | 0 | 0 | 0.167 |
| 20 | Treatments that afford only a brief period of time at the end of life are not worthwhile: they only prolong the pain for the family and/or friends of the patient | −2 | 0 | 1 | 0.747 |
| 21 | Prolonging the life of terminally ill patients only postpones death | −1 | 1 | 2 | 0.607 |
| 22 | Life is sacred, and if it is possible to preserve life, all efforts to do so should be made | −1 | -3 | 0 | 0.467 |
| 23 | I would not like my life to be prolonged just to keep me alive: respiratory assist is not life | 2 | 3 | 2 | 0.001 |
| 24 | All patients have the right to basic medical care, though clear limits should be established in terminal patients, since the drugs used are expensive and do not form part of basic care | 1 | 1 | −1 | 0.405 |
| 25 | It is important to offer life-prolonging treatments for the dying patient in order to allow him or her the time needed to reach a certain date or settle important issues, such as a family event or personal achievement | 2 | 0 | −1 | 0.408 |
| 26 | Treatments intended to prolong the life of terminal patients have less value as the patients become older | −2 | −1 | −2 | 0.075 |
| 27 | The treatment of terminal patients does not generate great health benefits, but the health system should focus on caring for those patients who need treatment most | 0 | −1 | 0 | 0.044 |
| 28 | An objective measure of healthcare expenditure control could be the legalization of euthanasia | 0 | 1 | −3 | 0.783 |
The three perspectives found in this study underscore the plurality of the points of view and the importance of furthering understanding of the issues referred to this topic in the critical care setting.
Point of view 1 (The importance of the family and environment in end of life decisions), predominant in the explored sample, represents a perspective in which the rights of patients to life and their environment are of paramount importance. Life is seen as precious, and so economical costs should not be spared, even though the benefits obtained may be considered limited. This opinion perspective considers that treatments should be applied if the patients and their families consider that such treatments will be of benefit. On the other hand, it is also considered that patients should be able to reject life-prolonging treatments if they so wish.
However, although it could be understood that people who agree with this view would not support a special policy referred to limitation of treatments at end of life, there may be doubts in this regard. Such doubts would not be due to a belief that these treatments should not be provided, but rather to disagreement with the overall cost-effectiveness analysis, as a guide to provision and restriction of access to any treatment for any patient requesting it.
Point of view 2 (The patient right to decide) appears to be a more contextualized and balanced perspective, since it supports the value of money in the treatment at end of life decisions – though this value is broader than the benefits for health and is defined in part by the preferences of society. This view holds that the treatments used to prolong life may be valuable and therefore should be provided, but that the value should be conditioned to quality of life.
It seems reasonable to assume that this opinion perspective is marked by efficiency. Patients do not have a right to all treatments – some of which may be excluded on the grounds of their profitability. It does not seem very likely that the interviewees defined under point of view 2 would support a policy placing priority on supportive treatments designed to prolong life without considering the quality of the latter.
Point of view 3 (Cost considerations in end of life dilemmas) is more consistent with a utilitarian perspective. The core principle here is to secure the greatest health gains for the largest number of patients through the efficient allocation of resources that are limited. This view considers restriction of the availability of cost-ineffective treatment to be acceptable.
While drawn from a relatively small sample, the factors identified reflect the intentionality of the interviewees and documents the points of view among the professionals in the ICU referred to ethical and cost issues in treatments at end of life.
Please cite this article as: Jiménez Alfonso A, Escudero Acha P, Ortiz-Lasa M, Chicote E, Dierssen-Soto T, González-Castro A. Tratamientos de soporte vital al final de la vida: costos y aspectos éticos. Punto de vista en una unidad de cuidados intensivos basado en la metodología Q. Med Intensiva. 2018;42:558–561.