To estimate the incidence of medication errors in Spanish intensive care units.
DesignPost hoc study of the SYREC trial. A longitudinal observational study carried out during 24h in patients admitted to the ICU.
SettingSpanish intensive care units.
PatientsPatients admitted to the intensive care unit participating in the SYREC during the period of study.
Main variables of interestRisk, individual risk, and rate of medication errors.
ResultsThe final study sample consisted of 1017 patients from 79 intensive care units; 591 (58%) were affected by one or more incidents. Of these, 253 (43%) had at least one medication-related incident. The total number of incidents reported was 1424, of which 350 (25%) were medication errors. The risk of suffering at least one incident was 22% (IQR: 8–50%) while the individual risk was 21% (IQR: 8–42%). The medication error rate was 1.13 medication errors per 100 patient-days of stay. Most incidents occurred in the prescription (34%) and administration (28%) phases, 16% resulted in patient harm, and 82% were considered “totally avoidable”.
ConclusionsMedication errors are among the most frequent types of incidents in critically ill patients, and are more common in the prescription and administration stages. Although most such incidents have no clinical consequences, a significant percentage prove harmful for the patient, and a large proportion are avoidable.
Estimar la incidencia de los errores de medicación en los servicios de Medicina Intensiva españoles.
DiseñoAnálisis post hoc del estudio SYREC. Estudio observacional longitudinal con seguimiento de 24h de una cohorte de pacientes ingresados en los servicios de Medicina Intensiva participantes.
ÁmbitoServicios de Medicina Intensiva españoles.
PacientesPacientes ingresados en los servicios de Medicina Intensiva participantes en el estudio SYREC durante el periodo de inclusión.
Variables principales de interésRiesgo, riesgo individual y tasa de errores de medicación.
ResultadosParticiparon 79 servicios de Medicina Intensiva, incluyéndose 1.017 pacientes, registrándose 591 (58%) con al menos un incidente. De estos, 253 (43%) presentaron al menos un incidente relacionado con la medicación. El número total de incidentes notificados fue de 1.424, de los cuales 350 (25%) fueron errores de medicación. El riesgo que tiene un paciente de sufrir un error de medicación por ingresar en un servicio de Medicina Intensiva es del 22% (RIQ: 8%, 50%), mientras que el riesgo individual es del 21% (RIQ: 8%, 42%). La tasa de errores de medicación fue de 1,13 errores de medicación por 100 pacientes/día de estancia. La mayoría ocurrieron en la fase de prescripción (34%) y administración (28%); el 16% produjeron daño al paciente y un 82% se consideraron «sin duda evitables».
ConclusionesLos errores de medicación constituyen una de las clases de incidentes más frecuentes en el paciente crítico, siendo más habituales en las fases de prescripción y administración. Aunque la mayoría no tienen consecuencias clínicas, un porcentaje significativo causan un daño al paciente, siendo en una elevada proporción evitables.
It is now recognized that providing medical care entails excessive risks compared with other activities or even with other situations considered to pose risks. In addition to the personal patient health consequences of such excessive risks, mention must be made of their important economic and social impact. Consequently, the identification and prevention of these risks constitute a priority concern for the quality policies of healthcare systems, with implication of the health authorities and organizations of many developed countries, including Spain,1 in addition to international organizations such as the European Union, the European Council, and the World Health Organization (WHO).2
In this context, reference multicenter studies have been made in different countries with the purpose of globally analyzing the adverse events (AEs) associated with medical care in hospitals–the estimated incidence varying between 4 and 17%. These studies have found problems related with the use of drugs to be one of the most frequent types of AEs.3
In Spain, the National Study on Adverse Effects (Estudio Nacional de Efectos Adversos, ENEAS 2005) confirmed these results. Approximately 10% of the patients reporting to hospital presented AEs, and drugs were likewise the most frequent cause (37.4%). Furthermore, of these events, a large proportion (34.8%) were avoidable.4
In relation to medication use, it must be remembered that in addition to the intrinsic risk of adverse reactions when used under appropriate conditions, drug substances also cause many AEs as a consequence of failure or error during their clinical use. Such events are referred to as “medication errors” (MEs).
In the context of “safe drug use”, it is stressed that in order to guarantee patient safety, error-proof drug utilization systems must be developed, with the adoption of measures to ensure that the risk is minimized, or at least to ensure that any such errors do not cause patient harm.
The problem is particularly important in critically ill patients, where drug substances constitute one of the main management resources. The fact that many of the drugs are considered to pose a high risk and are administered via the intravenous route, together with the severity and complexity of these patients, and the need for optimum communication among the different professionals, all contribute to increase the risk of AEs.5–8
In Spain there is little information available on AEs in the critical care setting, and there are even fewer data referred to medication-related AEs. For this reason, a collaboration agreement was established between the Spanish Ministry of Health and the Spanish Society of Intensive Care Medicine (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC) for conducting the multicenter “Safety and Risk in the Critical Patient” (“Seguridad y Riesgo en el Enfermo Critico”, SYREC) trial, with the aim of establishing the incidence of AEs and of no-harm incidents (NHIs), classifying them and evaluating their impact and avoidability. The results of this trial have recently been published.9
The objectives of this study were to estimate the incidence of medication-related NHIs and AEs in the Spanish Intensive Care Units (ICUs), and to analyze their characteristics, severity and avoidability, based on the findings of the SYREC trial.
Patients and methodsDesignA longitudinal observational study with 24h of follow-up was carried out, involving a cohort of patients admitted to the ICUs participating in the post hoc study of the SYREC trial.
Inclusion criteriaThe study comprised all patients admitted to the participating ICUs during the observation period, including those admitted, those discharged, and those who died during the 24h of follow-up. We included the NHIs and AEs that occurred, were detected and reported during the observation period in the Unit, as well as those incidents and events occurring outside the Unit but which represented the reason for admission to the latter.
Variables and measurementsPrimaryIncidence of MEs (risk, individual risk and rate).
SecondaryRelated to the hospital and the ICU: number of hospital beds, number of beds in the ICU, type of Unit (clinical, surgical, coronary, traumatologic, polyvalent, pediatric, others), degree of occupation and work load quantified by means of the “Nine Equivalents of nursing Manpower use Score” (NEMS).10
Related to the patient: age and sex.
Characteristics of the ME: process or step in the therapeutic chain in which the error originated and type of error according to the ME classification of the Ruiz-Jarabo group.11
Severity of the ME: this was assessed based on an adaptation of the ME classification of the Ruiz-Jarabo group.11 The changes introduced affected categories A and B, which were merged. Because of the difficulties sometimes found in assessing the consequences of the incident, we added a new category: category D (Table 1).
Medication error (ME) severity categories (adapted from Ruiz-Jarabo).11
| Category | Definition |
| A | Circumstances or situations capable of producing an incident, but which are detected and resolved before they are able to affect the patient |
| B | The incident affects the patient but causes no harm. No monitoring or intervention is needed |
| C | The incident affects the patient and causes no harm, but monitoring and/or intervention is needed to confirm that no harm has been caused |
| D | The incident causes harm that is impossible to determine |
| E | The incident contributes to or causes temporary (reversible) patient harm and requires intervention |
| F | The incident contributes to or causes temporary (reversible) patient harm and requires or prolongs hospital admission |
| G | The incident contributes to or causes permanent (irreversible) patient harm |
| H | The incident proves life-threatening for the patient, and intervention is needed to ensure survival |
| I | The incident contributes to or causes patient death |
Source: Otero López, et al.11
Avoidability of the ME: in accordance with assessment as established by the observer, NHIs and AEs were classified as totally avoidable, possibly avoidable, possibly unavoidable and unavoidable.
ProcedureAll Spanish ICUs (220 in total) were invited to participate through the SEMICYUC website, by e-mail and conventional mail. One hundred Units accepted, of which 21 finally did not complete the study and were thus excluded. With the purpose of standardizing the data collection criteria, two coordinators were assigned in each Unit–a physician and nurse–and received a document with the study design and instructions, as well as supporting and training material for distribution among all the professionals of the Unit before the start of the observation period.
For data collection we developed a questionnaire that was distributed in paper format. On the day of the study all the physicians, nurses and auxiliary personnel completed the corresponding questionnaires on a voluntary and anonymous basis. The coordinators of each center checked correct completion of the questionnaires and converted them to electronic (digital) format for submission to the principal study investigators by e-mail.
Data collection quality controlAll the reported incidents were individually reviewed by the principal study investigators. A consensus meeting was then held to examine the discrepancies and decide their inclusion or exclusion, as well as to reclassify those data which were considered to have been wrongly classified.
Statistical analysisThe univariate analyses included the absolute frequency measures for each center, i.e., number of patients, total number of MEs, NHIs, AEs, and the rest of the study variables. As relative frequency measures we calculated the risk (cumulative incidence) and the rate (incidence density) for each ME, NHI and AE. Table 2 describes the definitions used.
Definitions.
| Term | Definition |
| No-harm incident (NHI) | An incident causing no harm to the patient, either because it does not affect the patient or because it lacks consequences |
| Adverse event (AE) | Any unforeseen and unexpected incident reported by the professionals and that has caused harm or death as a consequence of medical care, and is not related to the course or possible complications of the patient background disease |
| Medication error (ME) | Any NHI or AE detected and reported by the professional, related to the medication |
| Risk (cumulative incidence) | It is calculated by dividing the number of MEs, NHIs or AEs by the total patients meeting the inclusion criteria. The parameter is expressed as a percentage and reflects the probability of suffering ME, NHI or AE as a result of having been admitted to the ICU |
| Individual risk | It is calculated by dividing the number of patients with at least one ME, NHI or AE by the total of patients included in the study. The parameter is expressed as a percentage and reflects the probability of suffering at least one ME, NHI or AE as a result of having been admitted to the ICU |
| Rate (incidence density) | It is calculated by dividing the number of MEs, NHIs or AEs by the total days of stay in the ICU. The parameter is expressed as the number of MEs, NHIs or AEs per 100 patients/day of stay in the ICU |
Qualitative variables were reported as frequency distributions. As central tendency measures for the quantitative variables we used the mean and standard deviation (SD) as a measure of dispersion, or the median and interquartile range (IQR) in the case of asymmetrical distributions.
In the bivariate analyses, use was made of the chi-squared test to explore possible associations between qualitative variables. Differences in means in turn were contrasted using the Student t-test for independent samples, or analysis of variance (ANOVA) for more than two means when the variables showed a normal distribution, following evaluation of the homogeneity of variances. In the case of asymmetrical distributions we used the median test as hypothesis contrasting test. Statistical significance was considered for p < 0.05.
The data obtained were entered in a MS Access database, followed by statistical processing with the SPSS version 15.0 statistical package.
Confidentiality and ethical aspectsThe confidentiality and anonymity of the information obtained in relation to the patients, professionals and ICUs participating in the study were observed at all times. The results of this study are not binding for the professionals or for the patients in any direct way, and both the positive and the negative results have been published. Since the study was of an observational nature, with no interventions of any kind, the obtainment of informed consent was not considered necessary. Each ICU was responsible for obtaining the pertinent permissions at local level.
ResultsSeventy-nine ICUs pertaining to 76 hospitals participated in the study. A total of 84% of the participating ICUs belonged to large or medium sized hospital centers. In relation to the type of Unit, most were polyvalent ICUs, particularly in the small and medium-sized hospitals (Table 3). Mean ICU occupation on the day of follow-up was 80% (IQR 64–99%). There was no statistically significant association between this variable and the size of the hospital.
Number of participating ICUs according to hospital size, type and size of ICU and number of cases contributed.
| Hospital size (beds) | Participating ICUs (% of the total) | % of polyvalent ICUsa | ICU beds in 2006 (mean) | Patients included on the day of the study | Patients with incidents | Number of incidents | No. NHIs | No. AEs |
| Small (≤200) | 13 (16) | 99 | 7 | 88 | 45 | 115 | 85 | 30 |
| Medium (201–499) | 34 (43) | 88 | 12 | 367 | 219 | 513 | 341 | 172 |
| Large (≥500) | 32 (41) | 81 | 18 | 562 | 327 | 796 | 517 | 279 |
| Total | 79 (100) | 1017 | 591 | 1424 | 943 | 48 |
AE: adverse event; NHI: no-harm incident; ICU: Intensive Care Unit.
The nursing work load as rated with the NEMS was analyzed in the 65 hospitals for which such information was available. A statistically significant association was observed between the mean work load and the size of the hospital, with greater work loads in large hospitals than in small centers.
A total of 1017 patients were included in the study. Of these, 591 (58%) registered at least one incident [381 (64.5%) males and 210 (35.5%) females]. Among the mentioned 591 patients, 253 (43%) suffered at least one ME. The mean age of the males was 61.52 years (SD 16.38), versus 61.84 years (SD 17.35) in the case of the females. The overall mean age was 61.63 years (SD 16.72). There were no statistically significant differences in terms of incidence between males and females. Likewise, the percentage of patients with MEs was similar, independently of the size of the hospital (p = 0.34).
A total of 1424 incidents were reported. Of these, 350 (25%) were medication-related, and represented the most frequently reported type of incidents. Table 4 shows the results corresponding to risk, individual risk and rate for the reported MEs, NHIs and AEs.
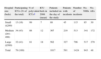
Risk, individual risk and ME, NHI and AE rates.
| Risk (%) | Individual risk (%) | Rate (per 100 patients/day) | ||||||
| Median | P 25 | P 75 | Median | P 25 | P 75 | Median | P 25 | P 75 |
| ME (n=350) (100%) | ||||||||
| 22 | 8 | 50 | 21 | 8 | 42 | 1.13 | 0.38 | 2.74 |
| NHI (n=294) (84%) | ||||||||
| 17 | 0 | 50 | 14 | 0 | 33 | 0.77 | 0.00 | 2.10 |
| AE (n=56) (16%) | ||||||||
| 0 | 0 | 9 | 0 | 0 | 9 | 0.00 | 0.00 | 0.44 |
AE: adverse event; ME: medication error; NHI: no-harm incident.
Regarding the characteristics of the MEs according to the process or step in the therapeutic chain in which they originated, those occurring in the prescription phase were the most frequent (34% of all cases), followed by administration-related MEs (28% of the total reported MEs) (Table 5).
Process or phase of the therapeutic chain in which the error is detected.
| Process or phase of the therapeutic process | ||||||
| NHI | AE | ME | ||||
| n | % | n | % | n | % | |
| Prescription | 102 | 35 | 17 | 30 | 119 | 34 |
| Transcription | 51 | 17 | 7 | 12 | 58 | 17 |
| Dispensation | 42 | 14 | 10 | 19 | 52 | 15 |
| Preparation | 11 | 4 | 1 | 2 | 12 | 3 |
| Administration | 81 | 28 | 16 | 28 | 97 | 28 |
| Monitorization | 7 | 2 | 5 | 9 | 12 | 3 |
| Total | 294 | 100 | 56 | 100 | 350 | 100 |
AE: adverse event; ME: medication error; NHI: no-harm incident.
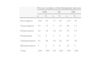
Considering the possible consequences of the MEs based on the classification of severity, 83% were reported as NHIs principally corresponding to categories A and B (Table 6). Medication errors related to prescription, transcription, dispensation and administration were the most frequent types resulting in NHIs. The preparation and monitorization errors showed no significant differences in frequency between NHIs and AEs.
Medication error severity and avoidability.
| ME severity category (n=350) (100%) | ||||||||
| NHI (n=294) (84%) | AE (n=56) (16%) | |||||||
| A | B | C | D | E | F | G | H | I |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| 102 (29.1) | 154 (44.0) | 38 (10.9) | 36 (10.3) | 14 (4.0) | 1 (0.3) | 0 (0.0) | 4 (1.1) | 1 (0.3) |
| ME avoidability | |||||||
| NHI (n=294) | AE (n=56) | ||||||
| Totally avoidable | Possibly avoidable | Possibly unavoidable | Totally unavoidable | Totally avoidable | Possibly avoidable | Possibly unavoidable | Totally unavoidable |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| 255 (86.7) | 34 (11.6) | 4 (1.4) | 1 (0.3) | 33 (58.9) | 19 (33.9) | 1 (1.8) | 3 (5.4) |
AE: adverse event; ME: medication error; NHI: no-harm incident.
Lastly, the reported MEs were predominantly regarded as “totally avoidable” (82%) compared with the rest of the avoidability categories. In turn, 98% of the NHIs and 93% of the AEs were regarded as “totally avoidable” or “probably avoidable” (Table 6).
DiscussionThe ICU participation rate in our study (33%) is similar to or even greater than in other national multicenter studies carried out to date.12,13 This may reflect a growing interest in recent years in knowing the true situation of Spanish ICUs regarding patient safety.14
Among other contributing factors, the appearance of ME in the ICU is conditioned by the severity of the patient and the work load of the nursing personnel, which is usually related to the number of beds.15 However, in our study, although there were no statistically significant differences in either the occupation rate or in the number of patients attended by each nurse, the NEMS was higher in the hospitals of larger size. Despite this observation, we found no statistically significant differences in ME incidence rate.
Perhaps the size of the hospital is not an appropriate characteristic for grouping ICUs. It therefore might be more interesting to seek a combination between the complexity of the patient and the work load of the professionals in order to classify the different types of Units with a view to conducting future studies of errors in critical patient care.
According to the results of our study, MEs were the most frequently reported incidents, representing 25% of the total. These findings are consistent with those reported by the ENEAS study in Spain, where the largest proportion of AEs detected in the hospital setting were likewise related to medication.4
In a more specific setting such as the ICU, Valentin et al., in an international multicenter study with a methodological design similar to our own, confirmed that MEs are among the most frequently reported incidents.16 It should be noted that the mentioned study differed from ours in relation to the types of MEs reported, since only the most common errors were taken into account, i.e., those that occur in the prescription and administration phases. In contrast, our study included all MEs detected in any phase of the therapeutic chain.
The “Adverse Drug Event Prevention Study”,7 a reference publication on MEs in hospitalized patients combining review of the case histories with voluntary declaration of AEs, explains the high incidence of MEs in the ICU as a consequence of the fact that critical patients receive twice as many drugs as the rest of patients. Such findings have been confirmed by Cullen et al.8
Other reasons that would account for these results are the continuous changes in the clinical condition of the patients, requiring modifications and dose adjustments; the numerous treatments received (many of which are considered to imply high risk); use of the intravenous route as the most common administration route; and the fact that in many cases the patients are under the effects of sedation, which prevents them from detecting healthcare personnel errors by themselves.7,8
However, the results derived from studies of this kind are highly variable, and such variation may be influenced by the definition of ME used in the investigation; the detection method used to determine this type of incident; the pharmacotherapeutic groups involved; the evaluated phase of the process or chain; and the inclusion or exclusion of the different administration routes employed. All this makes the comparison of such studies difficult.16,17 In this context, the findings can range from 1.2 MEs per 1000 patients/day when voluntary declaration is considered to 106 MEs per 1000 patients/day when evaluating errors related to continuous perfusions, or 947 MEs per 1000 patients/day when evaluating errors in the prescription phase.18,19
It is well known that MEs can occur in any phase of the therapeutic process,17 although they are more frequent during prescription and administration. Our study, with rates of 34% and 28% in these two phases, respectively, confirms the results obtained by other authors.20–24
It was not the aim of our study to analyze the causes of ME, since the data collection form was not specifically designed for this purpose. However, in the same way as in the study published by Ridley et al., it should be noted that most of the recorded prescription errors were attributable to ambiguous instructions, incorrect nomenclature, and illegible writing,20 while the most frequent situations referred to administration errors were omissions and delays in the timing of administration. Similar data have been reported by Valentin et al.25
Regarding the definition of severity, the lack of appropriate scales makes it even more difficult to establish a uniform definition, and therefore to establish comparisons with other studies. However, most studies report a high rate of NHIs.26,27 In our case the observed rate was even higher: 18 NHIs per 100 patients/day, representing 84% of all MEs (Table 6).
As in any voluntary declaration study, the professionals might feel intimidated to report cases of severe harm or injury in which they themselves are implicated. However, it should be underscored that in our study there were 51 reports of MEs (14%) that caused reversible patient harm and 5 reports of MEs (4%) that caused permanent damage–including one case resulting in patient death.
Regarding avoidability, the MEs were mostly considered to be “totally avoidable”, compared with the rest of possible avoidability categories. In the same way as in other studies,26–28 the confirmed fact that MEs are mostly avoidable (93% and 98% of the AEs and NHIs, respectively, were avoidable in our study) should cause us to reflect upon the advisability of adopting strategies designed precisely to avoid such situations. The above considerations point to the need for furthering our knowledge of ME and its epidemiology in the critical patient. Only a detailed analysis of the problem will allow us to define strategies capable of ensuring safer medication use.
Among the main limitations of our work, it must be underscored that this has been a descriptive study, and we are therefore unable to confirm any hypotheses referred to associations between variables. Any possible associations will have to be confirmed in posterior analytical studies.
Under-reporting is a limitation inherent to studies that use a voluntary and anonymous reporting system as a tool for data collection, and may be due to a lack of knowledge of what needs to be reported, a lack of awareness that an error has been made, or fear of reprisals. This aspect may have influenced our study, though we consider that there have also been other factors that have clearly conditioned reporting, such as the fact that the study results may have been influenced by the selection bias inherent to those studies in which participation is voluntary. In this context, it is possible that participation in the study was more likely on the part of those hospitals with greater awareness and motivation referred to patient safety, and therefore more inclined to report. Having a medical and nursing coordinator in each participating hospital, and the promotion of professional training may have contributed to increase reporting. On the other hand, the short data collection period involved (24h) might also have favored involvement among the professionals, motivating them to report incidents. In view of the above, we consider that, overall, our study favored the reporting of incidents.
It also must be commented that the SYREC trial was not specifically designed for the detection and reporting of MEs,9 and that consequently the recorded incidence may have been less than would be expected from a study specifically designed for that purpose. Furthermore, in most of the reported MEs the implicated drug was not specified, since the data collection form only required specification of the phase of the therapeutic process or chain in which the incident occurred. For this reason it is not possible to perform a more rigorous analysis of the pharmacotherapeutic groups most often implicated in ME – in contrast to other studies found in the literature.22,23
Another source of bias to be taken into account in studies of this kind, and which may have influenced the number of reported MEs, is the so-called Hawthorne effect, consisting in our case of the adoption of safer medical practices on the day of the study because the professionals feel themselves to be watched.
The classification of the incidents and their consequences contains subjective elements which in our study could be augmented by the fact that all the professionals were enrolled as reporters of incidents–a situation that favors inter-observer variability. The prior basic training does not allow us to guarantee sufficient experience for correctly categorizing the incidents, and concordance analyses moreover were not made. The use of pre-established definitions and posterior quality control, with a review of all the incidents by the principal investigators of the study, have attempted to minimize this limitation.
Lastly, the short follow-up period, which limits the information on the middle-term consequences of the detected AEs and precludes the detection of AEs whose consequences become manifest only days later, may have caused some AEs to go undetected, underestimating the severity and therefore influencing the results.
Considering the above limitations, the main contribution of this study has been the obtainment of information on the MEs that affect patients admitted to Spanish ICUs. Although there are reference publications corresponding to different countries, epidemiological studies in our own context are also needed to evidence that our ICUs suffer the same safety problems–thereby helping to increase awareness of the importance of a problem which has received little attention in our setting, and which therefore may have been underestimated to date.
In conclusion, medication error can be regarded as one of the most frequent incidents in critical patients, and is more common in the drug prescription and administration phases. Although most such errors have no clinical consequences, a significant percentage cause patient harm, and a large proportion of them are moreover avoidable. Specific strategies therefore should be adopted to ensure safe drug use in the critical care setting.
Financial supportThis study was carried out thanks to a collaboration agreement between the Spanish Ministry of Health and the Spanish Society of Intensive Care Medicine (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC).
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors of the study thank the coordinators of the participating ICUs for the support provided in carrying out this study.
Cánovas Robles J, Perales Pastor R, Hospital General Universitario de Alicante (Alicante); Sánchez Ortega D, Serrano Calvache JA, Hospital de Torrecárdenas (Almería); De Rojas Román JP, Ramos Carbonero Y, Hospital Comarcal de Antequera (Antequera); Gutiérrez Fernández MJ, Fernández Álvarez V, Hospital San Agustín (Avilés); Umaran Sarachu MI, Monguillo Martiregui MJ, Hospital de Cruces (Baracaldo); Fernández Dorado F, Figueras Coloma E, Centro Médico Delfos (Barcelona); Morillas Pérez J, Portillo Jaurena E, SCIAS-Hospital de Barcelona (Barcelona); Sánchez Segura JM, Sola Sole N, Hospital Santa Creu i Sant Pau (Barcelona); Zavala Zegarra E, Cirerea A, Hospital Clínic - UCI Quirúrgica (Barcelona); Vázquez Sánchez A, Abad Peruga V, Hospital del Mar (Barcelona); Robles González A, Borja García MI, Hospital Vall D’Hebron-Traumatología (Barcelona); Bellot Iglesias JL, Martínez Molina M, Hospital de Baza (Baza); Romero Pellerrejo J, Campillo Temiño C, Complejo Hospitalario de Burgos (Burgos); Martínez Hernández J, Alarcón Simarro N, Hospital Santa María del Rosell (Cartagena); Álvaro Sánchez R, Bernat Adell A, Hospital Universitario Asociado General de Castelló, (Castelló); Molina Domínguez E, Ortega Carnicer J, Hospital General de Ciudad Real (Ciudad Real); Alcalá López A, Pastor M, Hospital General Universitario de Elche (Elche); Palomeque Rico A, Nicolás Zambudio G, Hospital Sant Joan de Deu (Espluges); Alonso Ovies A, Balugo Huertas S, Hospital de Fuenlabrada (Fuenlabrada); Audicana Uriarte J, Sánchez Villamar AM, Hospital de Galdakao (Galdakao); Álvarez Villuendas A, Garfingou Llenas D, Hospital Dr. Josep Trueta (Girona); Roca Guiseris J, García R, Hospital Virgen de las Nieves (Granada); Fernández del Campo R, Buendía F, Hospital de Hellín (Hellín); Bartual Lobato E, García Verdejo JA, Hospital Can Misses (Ibiza); Verduras Ruiz MA, Rodrigo Frontelo R, Hospital Severo Ochoa (Leganés); Pavía Pesquera MC, Pardos Peirós E, Hospital San Pedro (Logroño); Blanco Pérez J, Murado Bouso AM, Hospital Xeral-Calde Lugo (Lugo); Gómez Tello V, del Pozo Y, Clínica Moncloa (Madrid); Reyes García A, Toledano Peña J, Hospital Universitario de la Princesa (Madrid); Ramos Polo J, Suay Ojalvo C, Hospital Clínico San Carlos (Madrid); Menéndez de Suso JJ, Segovia Gaitán M, Hospital San Rafael (Madrid); Sáenz Casco L, Andrés Sarriá M, Hospital Central de la Defensa Gómez Ulla (Madrid); Jiménez Lendínez M, Romero C, Hospital Universitario La Paz (Madrid); Arias Verdú MD, García Santana JL, Hospital Parque San Antonio (Málaga); Arboleda Sánchez JA, Velasco Bueno JM, Hospital Costa del Sol (Marbella); Solsona Perlasia M, Vilalta Llibre M, Consorci Sanitari del Maresme (CSdM) (Mataró); García Fernández AM, Morales Adeva L, Hospital de Mérida (Mérida); Galdos Anuncibay P, Arias Castro I, Hospital General de Móstoles (Móstoles); Gómez Ramos MJ, Cevidanes M, Hospital General Universitario Reina Sofía (Murcia); Martínez Fresneda M, Banacloche Cano C, Hospital Virgen de la Arrixaca (Murcia); Carrillo Alcaraz A, Peñalver F, Hospital Morales Meseguer (Murcia); Iglesias Fraile L, Álvarez Méndez B, Hospital General de Asturias (Oviedo); Rialp Cervera G, Bestard Socías C, Hospital Son Llàtzer (Palma de Mallorca); Rodríguez Albarrán F, Ballester Belcos R, Clínica San Miguel (Pamplona); Ramos Castro J, Herranz Ayesa MV, Hospital Virgen del Camino (Pamplona); Martínez Urionabarrenetxea K, Elizondo Soto A, Hospital de Navarra (Pamplona); Gil Cebrián J, Delgado Poullet N, Hospital Universitario Puerto Real (Puerto Real); Prieto Valderrey F, Nieto Galeano J, Hospital Santa Bárbara (Puertollano); Rovira Angles C, Cerrillo E, Hospital Universitario Sant Joan de Reus (Reus); Domínguez López S, Malnero López M, Hospital Valle del Nalón (Riaño); Baigorri González F, Jam Gatell R, Hospital de Sabadell-Corporació Parc Taulí (Sabadell); Lacueva Moya V, Hernández Santamaría F, Hospital de Sagunt (Sagunto); González Robledo J, Coca Hernández MA, Hospital Universitario de Salamanca (Salamanca); Azkárate Ayerdi B, Marcos A, Hospital Donosita (San Sebastián); Rull Rodríguez VE, Morras Pineda B, Complejo Hospitalario de Soria–Hospital de Santa Bárbara (Soria); Gilavert Cuevas MC, Aragonés M, Hospital Joan XXIII (Tarragona); Jurado Castro MT, Bell Ribatallada M, Hospital de Terrasa (Terrasa); Pérez-Pedrero Sánchez-Belmonte MJ, Pinilla López A, Hospital Virgen de la Salud (Toledo); Vázquez Casas JR, Herrero Gómez E, Hospital Verge de la Cinta (Tortosa); Soto Ibáñez JM, Romero Morán MA, Hospital Universitario Dr. Peset (Valencia); García Galiana E, Fernández Martínez A, Fundación Instituto Valenciano de Oncología (Valencia); Domínguez Quintero LA, Acebes Sancho BE, Domínguez Quintero LA, Palencia García MA, Hospital Río Hortega–Polivalente (Valladolid); Tizón Varela AI, de Castro Rodríguez P, Complexo Hospitalario Universitario de Vigo–Hospital Xeral Cíes (Vigo); Manzano Ramírez A, Ruiz de Ofenda E, Hospital Santiago Apóstol (Vitoria); Marcos Gutiérrez A, Larruscain León MV, Hospital Virgen de la Concha (Zamora); Temiño Palomera S, Lasheras Palomero L, Mutua de Accidentes de Zaragoza (Zaragoza); Gutiérrez Cía I, Moreno MA, Hospital Clínico Universitario Lozano Blesa–UCI Quirúrgica (Zaragoza); Tirado Angles G, González Caballero M, Hospital Royo Villanova (Zaragoza); Valero García R, Casa Venta J, Hospital Universitario Miguel Servet–Coronaria (Zaragoza); García Mangas P, Mahave Carrasco R, Hospital Universitario Miguel Servet–Polivalente (Zaragoza); Olmos Pérez F, Villabona Resano J, Hospital Universitario Miguel Servet–Cirugía Cardiaca (Zaragoza); Williams L, Patiño Y, Centro de Especialidades Anzoátegui, Lechería (Venezuela); Margarit Ribas A, Flamarique Zaratiegui MT, Hospital Nostra Senyora de Meritxell, Escaldes-Engordany (Andorra); Ortega RA, Sánchez Reinoso J, San Juan Bautista, Catamarca (Argentina); Diosdado Iraola Ferrer M, Mora Pérez Y, Hospital Universitario Dr. Gustavo Aldereguía Lima, Cienfuegos (Cuba); Carrazana Ososrio V, Prieto Fuentemayor JR, Hospital Clínico-Quirúrgico Lucía Íñiguez Landín, Holguín (Cuba); Díaz Águila H, Companioni Sola Y, Hospital «Mártires de 9 de Abril», Sagua la Grande (Cuba); Morales Valderas A, Solís Sotero M, Hospital Universitario Arnaldo Milian Castro, Santa Clara (Cuba).
Please cite this article as: Merino P, Martín MC, Alonso A, Gutiérrez I, Álvarez J, Becerril F, et al. Errores de medicación en los servicios de Medicina Intensiva españoles. Med Intensiva. 2013;37:391–399.