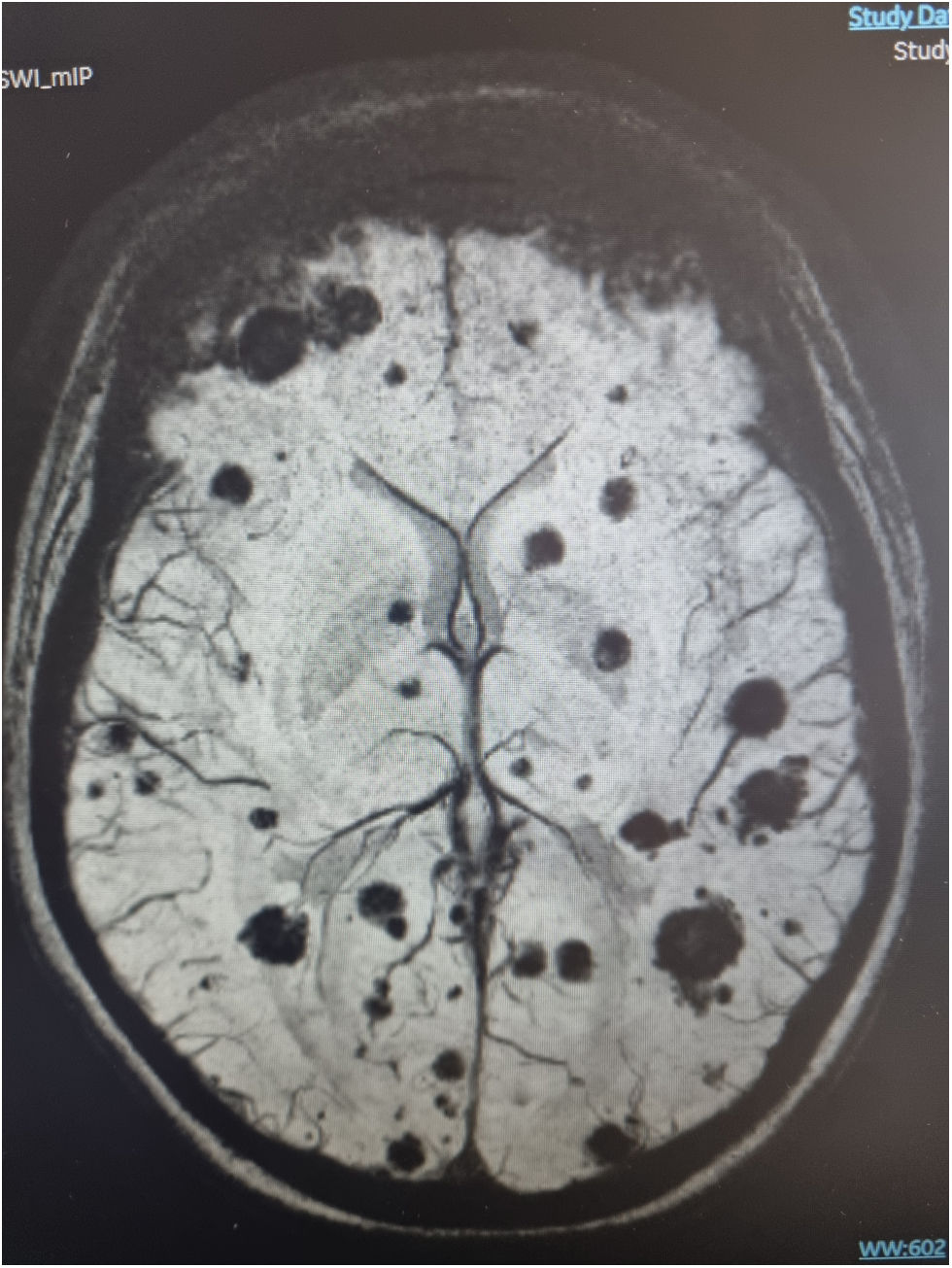
A 23-year-old woman presents with a severe acute liver failure syndrome of unclear etiology, initially treated with a 1-month regimen of corticosteroids due to suspected autoimmune causes. She subsequently experiences neurological deterioration, leading to a cranial CT scan that reveals multiple space-occupying lesions. The full-body CT performed reveals the presence of microabscesses in abdominal organs, and the cranial MRI reveals the presence of numerous supra- and infratentorial focal signal alterations with central hemorrhagic components and areas of diffusion restriction at the periphery. After contrast administration, there is fine peripheral enhancement, all of it consistent with septic embolic encephalitis. Blood cultures and transesophageal echocardiography rule out suspected endocarditis. A lumbar puncture was not feasible due to thrombocytopenia. Ultimately, Aspergillus fumigatus is identified via PCR in bronchoalveolar lavage, which turned out positive. Antifungal treatment is initiated but with poor clinical progression, and the patient ultimately develops brain death (Fig. 1)
FundingNone declared.