The medical indications of tracheostomy comprise the alleviation of upper airway obstruction; the prevention of laryngeal and upper airway damage due to prolonged translaryngeal intubation in patients subjected to prolonged mechanical ventilation; and the facilitation of airway access for the removal of secretions. Since 1985, percutaneous tracheostomy (PT) has gained widespread acceptance as a method for creating a surgical airway in patients requiring long-term mechanical ventilation. Since then, several comparative trials of PT and surgical tracheostomy have been conducted, and new techniques for PT have been developed. The use of percutaneous dilatation techniques under bronchoscopic control is now increasingly popular throughout the world. Tracheostomy should be performed as soon as the need for prolonged intubation is identified. However a validated model for the prediction of prolonged mechanical ventilation is not available, and the timing of tracheostomy should be individualized. The present review analyzes the state of the art of PT in mechanically ventilated patients – this being regarded by many as the technique of choice in performing tracheostomy in critically ill patients.
Las indicaciones para la realización de la traqueotomía se pueden resumir en: 1. obstrucción de la vía aérea superior, 2. prevención del daño laríngeo y de la vía aérea alta por intubación prolongada en pacientes sometidos a ventilación mecánica prolongada, y 3. permitir un fácil acceso a la vía aérea para la eliminación de secreciones. Desde 1985 la traqueotomía percutánea (TP) se ha ido consolidando como la técnica para establecer una vía aérea quirúrgica en los pacientes que necesitan ventilación prolongada. Desde entonces, se han publicado diferentes estudios comparativos entre TP y traqueotomía quirúrgica, se han desarrollado nuevas modalidades de TP y el uso de las técnicas por dilatación con control endoscópico continúa extendiendo su popularidad por todo el mundo. La traqueotomía debe realizarse tan pronto como se identifica la necesidad de tener un paciente ventilado de forma prolongada, sin embargo no hay modelos para predecir tal situación y el momento para su realización debe individualizarse. En el presente artículo analizaremos el estado actual de la TP en los pacientes ventilados mecánicamente, considerada para muchos la técnica de elección para la realización de la traqueotomía en el enfermo crítico.
Tracheostomy is one of the most common techniques used in the Intensive Care Unit (ICU). Although the procedure is assumed to be thousands of years old, modern tracheostomy was introduced with the description of surgical tracheostomy (ST) by Jackson in 1909.1 In that period, inflammatory or tumor processes causing airway obstruction were the main indication of the technique. With advances in the fields of surgery, critical care and positive pressure mechanical ventilation, tracheostomy received a new indication: prolonged mechanical ventilation. For years this was a feared technique, often associated with serious and event fatal complications; physicians therefore attempted to avoid the procedure, and patients remained intubated for weeks and even months.2 In 1985, Bishop et al.3 published an experimental study on the consequences of prolonged intubation, and that same year Ciaglia et al.4 described percutaneous dilatation tracheostomy (PDT), which proved simple, rapid and safe. Furthermore, the technique could be performed at the patient bedside, leading to a new way of viewing surgical access to the airway in the critically ill patient.
Types of percutaneous tracheostomyFive years after the description of PDT by Ciaglia et al.,4 Griggs et al.5 introduced tracheostomy using guide wire dilating forceps (GWDF) (Portex Limited, Hythe, Kent, United Kingdom). With this technique the tracheostoma is opened using blunt-tipped forceps (designed with a cannulated internal margin through which a metal guide wire can be inserted) previously advanced over the metal guide in the tracheal lumen. In 1998 the classical technique of Ciaglia was modified using a single dilator6 (Ciaglia Blue Rhino [CBR], Cook Critical Care, Bloomington, IN, USA). With respect to the original technique, this modification offered the advantage that the stoma is produced by a single dilatation, thereby avoiding the need for successive dilatations. Fantoni and Ripamonti7 in turn developed the translaryngeal technique (Mallinckrodt, Mirandola, Italy) – a complex system in which the stoma is made by exteriorizing a dilator from within the trachea, using a specially designed tracheostomy cannula and a rigid bronchoscope. In 2002, Frova and Quintel8 described the PercuTwist technique (Rüsch GmbH, Kernen, Germany), in which the tracheostoma is made using a rotation system. Another modification of the classical technique of Ciaglia was introduced in 2008 (Ciaglia Blue Dolphin [CBD], Cook Critical Care, Bloomington, IN, USA), involving dilatation performed by insufflating a balloon.9
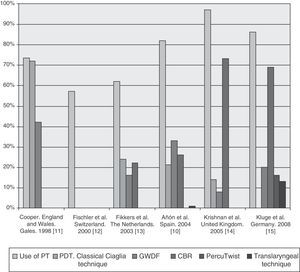
The techniques most widely used in Spain in the early years of the last decade were the Griggs technique, the Ciaglia PDT, and the Ciaglia Blue Rhino.10 At that time the balloon dilatation technique had not been developed, and the PercuTwist procedure was being introduced. An additional 5 European surveys have evaluated the use of percutaneous tracheostomy (PT) in the ICU, and their results are shown in Fig. 1.11–15
Indications and contraindications of percutaneous tracheostomyThe indications of tracheostomy can be summarized as follows: (1) need for airway permeation; (2) prevention of laryngotracheal damage caused by prolonged intubation; and (3) maintenance of adequate tracheobronchial hygiene, facilitating the aspiration of secretions in patients with spontaneous secretion clearing problems.
The classical contraindications of PT have been obesity, a short neck, gout or neck deformities, coagulation disorders (INR>1.5) or thrombopenia (platelet count<50,000/mm3), children under 16 years of age, the need to establish an emergency surgical airway, probable or confirmed cervical spine damage, previous neck surgery or tracheostomy, infection in the surgical zone, and high oxygen and PEEP requirements.16–18
As experience with PT has increased, so has clinician confidence with the technique, while the restrictions in high risk patients have decreased. Nevertheless, it must be taken into account that young children, cervical injury and infection of the surgical zone remain absolute contraindications. Some risk groups and the pediatric population deserve special mention.
ChildrenToursarkissian et al.19 evaluated PDT in 11 children and adolescents between 10 and 20 years of age, with good results. They recorded an intraoperative and a postoperative complication in the same patient that were easily recognized and treated, and in no case was tracheal stenosis observed in 8 decannulated patients during a follow-up period of 43±30 weeks. More recently, Raju et al.20 have compared ST with PT in pediatric trauma patients. The mean age of both groups was 14.2 and 15.5 years for ST and PT, respectively. No significant differences were observed, and the authors concluded that PT is a safe option in older children.
However, the characteristics of the trachea in children may make them more susceptible to certain serious complications. There is not enough experience in this population, and it is ethically questionable to conduct randomized trials to evaluate a technique in which the risks of a learning curve would have to be accepted in a population (pediatric patients) for which it was not designed.21,22 At this time there are no guides or recommendations warranting its application in children.
ObesityFew studies have examined the safety of PT in obese patients, and the existing data are moreover contradictory. Mansharamani et al.23 published their experience in 13 patients with a body mass index (BMI)>27kg/m2. They described a false passage and a case of balloon rupture, with no fatalities attributable to the technique. The latter was thus considered safe in this population. Byhahn et al.24 obtained different results in a cohort of 73 patients with BMI>27.5kg/m2 in which PT was performed under endoscopic control using one of the following methods: classical PDT, CBR and the translaryngeal technique. There were complications in 43% of the 73 patients classified as obese, versus in 18% of the 401 patients without obesity. A total of 9.6% of the obese subjects suffered serious complications (defined as problems with an impact upon morbidity and mortality), versus 0.7% in the other group. The serious complications in the obese patients included posterior tracheal wall damage and anterior esophageal tearing, as well as accidental decannulation.
Although obesity is currently not an absolute contraindication to PT, it is a condition that does require a number of precautions. Anatomical localization may prove more difficult in some cases, and longer tracheostomy cannulas are probably required in the last step of the technique. Successful performance of the procedure is conditioned by the degree of obesity, with the need for reasonable identification of the puncture zone; the experience of the medical team; and the safety measures adopted.
Previous tracheostomyPrevious tracheostomy has been a classical contraindication to PT. To date only one study involving a small sample and with a lack of follow-up has reported no serious complications with “retracheostomy” in 14 subjects. The authors defend the safety of the procedure.25 Although the technique is an attractive alternative to ST in these cases, its application must be conditioned to the characteristics of the patient and the experience of the team performing the procedure.
ThrombopeniaKluge et al.26 published the results of a retrospective study on the safety of PT using the Griggs technique in ventilated patients with platelet counts of under 50,000/mm3. The mean platelet count was 26,400/mm3, and the number of platelet units transfused before PT was 6±2.5. Only two patients (5%) suffered bleeding that required suturing after the procedure. Both presented prolongation of activated partial thromboplastin time due to heparin treatment. The authors concluded that the technique has a low complication rate when performed by experienced personnel, and provided prior platelet transfusion has been carried out. However, suspension of heparin infusion was considered necessary before performing the procedure. It should be noted that before the publication of the study by Kluge et al.,26 some studies had already considered that the contraindications related to coagulation disorders are conditioned to the possibility of correcting such disorders. The results obtained are important in that they offer information not previously available, reinforcing the relative nature of such contraindications.
High fraction of inspired oxygen and positive end-expiratory pressure requirementsHigh fraction of inspired oxygen (FiO2) and positive end-expiratory pressure (PEEP) requirements has been the exclusion criteria in different studies, with values that vary over a broad range. Once again, however, there are few studies on this subject, and no recommendations have been established. In order to evaluate the impact upon oxygenation of PDT under endoscopic guidance, Beiderlinden et al.27 compared the technique in two groups of patients with PEEP>10mmHg and with PEEP≤10mmHg. Oxygenation was not found to worsen one and 24h after performing PDT, and the authors did not experience changes in the patients with the greatest alteration in gas exchange. The authors therefore concluded that acute respiratory failure with high FiO2 and PEEP levels should not be regarded as a contraindication to PT.
Complications of percutaneous tracheostomyA number of reasons make it difficult to obtain a rigorous estimate of the perioperative complications of PT: (1) the baseline conditions of the patient may play a predisposing role; (2) the complications are directly conditioned to the degree of experience, which has been evaluated in only a few studies to date; (3) some of the more serious complications of PT can be avoided by adopting adequate safety measures, though these have not been widely used in the comparative studies; and (4) the definition of each event varies considerably among the different studies. In this regard, standardization of these aspects would allow us to obtain more objective and homogeneous information on the acute complications of the different types of PT. In this regard we propose the definitions of the complications of PT shown in Table 1, modified from Durbin.28
Proposed definitions for the perioperative complications of percutaneous tracheostomy (PT).
| Complication | Definition |
| Hypoxemia | SaO2 by pulseoximetry ≤90% during >30s |
| Severe hypoxemia | SaO2 by pulseoximetry ≤90% during >60s or ≤85% any duration |
| Loss of airway control | Failure to access airway for more than 20s |
| Bronchospasm | Bronchoconstriction related to performance of the technique |
| Mild arrhythmia | Bradycardia or tachycardia without effects upon blood pressure |
| Severe arrhythmia | Ventricular tachycardia, ventricular fibrillation, asystolia or any arrhythmia with hemodynamic impairment |
| Difficulty inserting the tracheostomy cannula | Need for more than two attempts to insert the cannula |
| Balloon rupture | Impossibility of keeping balloon insufflated as the result of maneuvering while performing the technique |
| Hypotension | Decrease in blood pressure of at least 20% with respect to baseline |
| Moderate hypotension | Hypotension requiring treatment with the infusion of <1000ml of fluids during the procedure |
| Severe hypotension | Hypotension requiring treatment with vasopressors or >1000ml of fluids during the procedure |
| Bleeding | Mild: bleeding that subsides with digital pressure and is estimated to be <20mlModerate: bleeding estimated to be >20mlSevere: bleeding with repercussion upon hematocrit (≥3 points), and requiring surgical repair or transfusion |
| Barotrauma | Mild: subcutaneous emphysemaModerate: mediastinal emphysemaSevere: pneumothorax |
| False passage | Dilatation or insertion of the tracheostomy cannula outside the tracheal lumen |
| Damage of the posterior tracheal wall | Damage of the posterior tracheal wall caused by the needle, guide or dilator |
| Tracheal tearing | Tracheal wall tearing during the dilatation procedure |
| Atelectasis | Total or partial lung collapse not present before the technique, and evidenced at postoperative control |
| Flexion of the metal guide | Guide cannot be moved into the tracheal lumen |
| Trapping of the metal guide | Metal guide cannot be removed |
| Failure in completing the technique | Need for a second (different) team to complete the technique, or need for ST to complete the procedure |
| Lateralization of the stoma | Stoma outside the anterior quadrant of the tracheal wall |
| Tracheal ring fracture | Tracheal ring rupture during any phase of the procedure |
| Death | Death related to complications of the technique |
ST, surgical tracheostomy.
Surgical tracheostomy has been the gold standard for comparison with PT. Table 2 shows the results of the randomized studies29–42 that have compared ST and PT (predominantly PDT). Only two studies found the incidence of intra- or postoperative complications to be significantly greater with PDT than with ST.
Comparative randomized studies between surgical tracheostomy (ST) and percutaneous tracheostomy (PT).
| ST/type of PT | n | Bleeding | Infection | Intraoperative complications | Postoperative complications | p | |
| Hazard et al.29 | ST/PDT | 46 | 4/1 | 8/1 | NA | 11/3 | <0.05 |
| Crofts et al.30 | ST/PDT | 53 | 3/3 | 1/0 | NA | 6/4 | NA |
| Friedman et al.31 | ST/PDT | 53 | 7/5 | 4/0 | 11/9 | 12/3* | 0.008* |
| Holdgaard et al.32 | ST/PDT | 60 | 36/9* | 19/3* | 26/19 | 30/7 | <0.01* |
| Porter and Ivatury33 | ST/PDT | 24 | 0/0 | 0/0 | 1/5 | 0/0 | NA |
| Gysin et al.34 | ST/PDT | 70 | 4/4 | 3/4 | 4/14* | 8/15 | 0.01* |
| Heikkinen et al.35 | ST/GWDF | 56 | 1/5 | 0/0 | 0/5 | 1/1 | NSa |
| Freeman et al.36 | ST/PDT | 80 | 2/0 | NA | NA | 2/0 | NDa |
| Massick et al.37 | ST/PDT | 100 | 0/2 | 0/1 | 1/4 | 1/9* | <0.05* |
| Melloni et al.38 | ST/PDT | 50 | 1/2 | 7/0* | 0/2 | 9/1 | <0.001* |
| Sustić et al.39 | ST/GWDF | 16 | 1/1 | 2/0 | 1/1 | 2/0 | NS |
| Wu et al.40 | ST/PDT | 83 | 4/3 | 3/1 | 1/4 | 7/3 | NS |
| Antonelli et al.41 | ST/TLT | 139 | 6/0 | 6/6 | 7/7 | 26/13* | 0.02* |
| Silvester et al.42 | ST/PDT | 200 | 1/4 | 14/4* | 2/5 | 14/13 | 0.04* |
GWDF, guide wire dilating forceps; NA, not available; NS, nonsignificant; TLT, translaryngeal tracheostomy; PT, percutaneous tracheostomy; PDT, percutaneous dilatation tracheostomy (classical Ciaglia technique); ST, surgical tracheostomy.
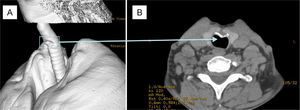
Few studies have focused on the late complications (some of which are inherent to tracheostomy, regardless of the technique used) of PT, and the existing publications moreover involve small samples due to the high in-hospital and middle-term mortality among critical patients susceptible to PT. This makes it difficult to obtain representative samples for study (Table 3).43–54 The most feared complications are fistula of the innominate artery, tracheomalacia, tracheoesophageal fistula and tracheal stenosis. Other less serious complications are tracheocutaneous fistula, hoarseness and/or voice changes, or esthetic alterations. In relation to the more serious complications, the following should be noted: (1) tracheal stenosis causes no symptoms until 50–75% of the lumen is obliterated, and most cases therefore can be subclinical (Fig. 2); (2) the mortality rate associated with fistula of the innominate artery is close to 100%, and the preventive measures include not performing tracheostomy too low, in order to avoid resting of the cannula on the artery, and avoiding excessive movements on the part of the patient; (3) a tracheoesophageal fistula may be produced when performing PT, secondary to posterior tracheal wall damage, or on a delayed basis as a consequence of excessive balloon insufflation or posterior wall damage caused by continuous trauma produced by the tracheostomy cannula tip; and (4) tracheomalacia is a result of damage to the tracheal cartilage, causing the trachea to become distensible, and in acute ventilated patients the tracheomalacia zone must be passed by introducing a longer tracheostomy tube while waiting definitive treatment.
Late complications of percutaneous tracheostomy (PT).
| Author/year/design | Type | n | Follow-up | Evaluation | Tracheal stenosis | Others | Surgical wound | Symptoms |
| Hill et al.43Prospective | PDT | 258/353a | 10±7 months | Interview and clinical evaluation | Stenosis requiring revision n=5 (2.3%) | Excessive granulation tissue in stoma: n=1 (0.4%) | Hoarseness: n=1 (0.4%)Dysphagia: n=1 (0.4%) | |
| Van Heurn et al.44Prospective | PDT | 66 | 16 months (3–39) | Tomography (n=54) | Stenosis >10% n=14 (26%) | Sore retraction | Voice changes: n=12 | |
| Law et al.45Not specified | PDT | 41 | Minimum 6 months after decannulation | LT | Stenosis >10% n=4 (9.7%) | No | ||
| Rosenbower et al.46Prospective | PDT | 55/95 | Minimum one year | Clinical (n=55) and LT (n=9) | Subglottic stenosis after decannulation (n=2)a | Tracheocutaneous fistula (n=1) | Minimum voice changes. Respiratory impairmenta | |
| Walz et al.47Prospective | PDT | 106 | 9.9±5.6 months | Conventional X-rays (2 planes) | Stenosis >10% n=46 (43.4%)Stenosis 50% n=4 (3.7%) (n=1 symptomatic)a | Breathing difficulty, stridora | ||
| Leonard et al.48Prospective | GWDF | 39/49 | 6 months | RFT (n=13) LT (n=10) | n=1 symptomatic tracheal stenosis before revision | Minimum voice changes. No respiratory impairment | ||
| Steele et al.49Retrospective | GWDF | 25 | >6 months | CAT | 0 | Tracheal dilatation, n=8 (32%) | Permanent hoarseness (n=2). Voice changes (n=9) | |
| Norwood et al.50Not specified | PDT | 100 | 30±25 months | CAT (n=48) and LT (n=38) | CAT: stenosis >10% n=15bLTcn=1 (10%) >50% | n=15 cosmetic revision of sore considered | Voice changes: 27%Persistent hoarseness: 2% | |
| Dollner et al.51Retrospective | GWDF | 19 | 17 months (r: 11–23) | LT | Stenosis >10%n=12 (63%)n=2 stenosis >25% | Cricoid cartilage damage, n=7 (32%) | No | |
| Fikkers et al.52Prospective | GWDF | 106/171 | 2.5 years (minimum: 14 months) | Laryngoscopy | Subglottic stenosis n=1 (0.9%) Required stent | Cosmetic problems n=10 (9.4%). Two required corrective surgery | Hoarseness or voice changes (n=9)-without anomalies at indirect laryngoscopyStridor: n=1 | |
| Carrer et al.53Prospective | n=181; PDT (n=48; 26.5%)/PercuTwist (133; 73.5%) | 141 | 3, 6, 12 months | Fibroscopy | Tracheal stenosis n=1 (0.7%) | Recurrent granuloma in stoma n=2 (1.4%) | ||
| Karvandian et al.54Prospective | PDT | 20/140 | 4 months | Fibroscopy and CAT | Subglottic stenosis n=17 (85%) | Tracheomediastinal fistula n=1 |
RFT, respiratory function tests; GWDF, guide wire dilating forceps; LT, laryngotracheoscopy; CAT, computed axial tomography; PDT, percutaneous dilatation tracheostomy (classical Ciaglia technique).
Finding (in the context of protocolized follow-up) in an asymptomatic patient 6 months after percutaneous tracheostomy using the Ciaglia Blue Dolphin technique. (A) Spiral CAT reconstruction showing anteroposterior displacement of the tracheal cartilage, and (B) causing 15% stenosis of the tracheal lumen.
Each type or modality of PT has its own characteristics, and this has led to the conduction of comparative studies in search of the safest option. However, these studies have been heterogeneous and with small samples. Table 4 summarizes the prospective and randomized studies published to date.55–64
Comparison between different percutaneous tracheostomy (PT) modalities. Prospective and randomized studies.
| Author/year | Type PT | EG | n | ETI time before PT | Bleeding | Pneumothorax or emphysema | Technical difficulty | Airway obstruction | Tracheal tearing | Tracheal ring fracture | CRA | False passage | AC | p |
| Nates et al.55 | PDT/GWDF | NA | 50/50 | 6/6.5 | 1/7 | – | 1.3/1.8a | 0/4 | – | – | – | 0/2 | 5/6 | 0.02b |
| Byhahn et al.56 | PDT/CBR | Yes | 25/25 | 7.5/7.2 | 1/0 | 1/0 | – | – | 2/0 | 2/9$ | – | – | 1/2 | <0.05$ |
| Johnson et al.57 | PDT/CBR | No | 25/25 | NA | 3/4 | – | 5/2 | – | – | – | – | – | 5/6 | NS |
| Van Heurn et al.58 | PDT/GWDF | No | 63/64 | 14.3/13.6 | 4/7 | – | 0/6 | – | – | – | – | 0/2 | – | 0.03c |
| Byhahn et al.59 | CBR/PTwist | Yes | 35/35 | 9.5/NA | 3/2 | 1/0 | 0/6* | – | 0/1 | 1/1 | 0/1 | 0/1 | 0/1 | <0.05* |
| Cantais et al.60 | GWDF/TLT | Yes | 53/47 | 18 | 12/2 | 1/1 | 0/11 | – | 1/2d | – | – | – | 0/7 | 0.001e |
| Ambesh et al.61 | CBR/GWDF | No | 30/30 | 9/8 | 1/5† | 1/3f | 2/9† | – | 2/3 | 9/0† | – | – | 2/0 | <0.05† |
| Añon et al.62 | CBR/GWDF | No | 27/26 | 17.4/20.3 | 2/1 | – | 0/3 | – | – | – | – | – | – | NS |
| Kaiser et al.63 | PDT/GWDF | No | 48/52 | 7/9 | 17/6 | 1/0 | – | 1/0g | – | – | – | 6/0 | 0.0001h0.008 | |
| Cianchi et al.64 | CBR/CBD | Yes | 35/35 | 2/2.5 | 12/24 | – | 3/10 | – | – | 2/3 | – | – | – | <0.01i0.02 |
AC, anesthetic complications; CBR, Ciaglia Blue Rhino; GE, endoscopic guide; GWDF, guide wire dilating forceps; ETI, endotracheal intubation; n, number of randomized patients; NA, not available; NS, nonsignificant; CRA, cardiorespiratory arrest; PTwist, PercuTwist; TLT, translaryngeal tracheostomy (Fantoni technique); PT, percutaneous tracheostomy; PDT, percutaneous dilatation tracheostomy (classical Ciaglia technique).
Anesthetic complications: loss of airway control, arterial hypotension, desaturation or arrhythmias.
Technical difficulty rated by the supervising physician: (1) easy, (2) some difficulty, (3) very difficult, (4) requires the professional of greatest experience, or the technique cannot be completed (p=0.01).
Three randomized studies have compared PDT versus GWDF. In a series of 100 patients, Nates et al.55 observed increased technical difficulty and a higher incidence of bleeding with GWDF – the balance of the global complications being favorable to PDT. Van Heurn et al.,58 in 127 patients (63 randomized to PDT and 64 to GWDF), likewise recorded a higher incidence of complications in the GWDF group. Although the authors specified that all the techniques were performed or assisted by experienced personnel, they described cannula insertion difficulties in 8 patients in the GWDF group – thus suggesting that discrete changes in the operating group could have avoided some of the observed complications. In a more recent comparative study, Kaiser et al.63 randomized 48 patients to PDT and 52 to GWDF. In this case, the incidence of minor and major complications was significantly greater in the PDT group than in the GWDF series. Of note is the high presence of certain complications such as bleeding in both groups, and a large number of anesthetic complications in the PDT group. This could have a number of explanations: (1) failure to use endoscopic guidance, which possibly could have contributed to avoid some of the described complications (damage to the posterior tracheal wall, loss of airway control); (2) strict definition of the complications (as could be the case of the definition of minor bleeding); and (3) lack of experience of the personnel performing the technique. The authors discard this latter factor, since the team was experienced with both techniques (at least 20 operations with each of them). Although many studies fail to mention the degree of experience of the physicians performing the procedure, it is difficult to say how many performed interventions suffice to guarantee extensive expertise, and the degree of experience is generally left to the authors to define.
Percutaneous dilatation tracheostomy versus Ciaglia Blue RhinoTwo studies have compared PDT with CBR. In one of them, Johnson et al.57 observed no significant differences between the two procedures in a series of 50 patients, while in the other study, likewise involving 50 patients, Byhahn et al.56 recorded 7 complications with PDT (3 of them of a serious nature) and a greater incidence of tracheal cartilage damage with CBR. They concluded that the latter is more applicable than PDT, since they recorded no serious complications with CBR.
Guide wire dilating forceps versus Ciaglia Blue RhinoTwo studies have compared GWDF with CBR. Ambesh et al.,61 in a sample of 60 patients, reported greater technical difficulty and bleeding with GWDF, as well as over-dilatation of the stoma. The patients randomized to CBR had a greater incidence of tracheal cartilage damage and elevated airway pressure. In our experience62 with 53 patients (27 randomized to CBR and 26 to GWDF), we observed no significant differences between the two techniques in terms of complications, though in coincidence with the findings of other authors,58 we recorded greater technical problems with GWDF – fundamentally referred to as difficulties in inserting the cannula.
Ciaglia Blue Rhino versus PercuTwistA randomized, prospective study of 70 patients has compared CBR with the PercuTwist technique.59 Greater technical difficulty was reported with the PercuTwist, together with two cases of tearing of the posterior tracheal wall. The authors acknowledged heterogeneous experience with the two techniques. Specifically, the team was familiarized with CBR, but had no prior experience with PercuTwist. It therefore can be affirmed that the study was carried out in the course of the learning curve of the PercuTwist technique – this representing a clear source of bias that limits the conclusions drawn.
Ciaglia Blue Dolphin versus Ciaglia Blue RhinoCianchi et al.64 compared CBR with CBD under endoscopic guidance in the context of a randomized prospective study of 70 critical patients in which the results were favorable to the former technique. The authors found CBR to be faster to perform, and with a lesser frequency of bleeding (mild tracheal mucosal bleeding evidenced by endoscopy 6h after the procedure), while insertion of the tracheostomy cannula proved more difficult with CBD. Their comparatively lesser familiarity with CBD may have influenced the results. Despite the observed differences, the authors concluded that CBD is indicated in the ICU. In view of the recent introduction of the technique, further randomized studies are needed, involving comparisons made by teams with equivalent experience in the use of both modalities.
MetaanalysesCabrini et al.65 have recently published a meta-analysis of all the randomized studies that have compared at least two PT techniques. They included 13 publications, of which 7 made use of endoscopic control. The authors found all the techniques to be equivalent, with the exception of the Fantoni technique, which was associated with more serious complications and with a greater need to convert to another tracheostomy technique compared with GWDF or CBR. The latter technique in turn was associated with fewer failures than PercuTwist, and with fewer mild complications than CBD or GWDF. They therefore concluded that CBR is the safest option and offers the highest success rate – though no recommendations for specific groups can be made. This has been the first meta-analysis to compare the most widely used PT modalities, though it is limited by the heterogeneous nature of the reviewed studies. One of the included studies was a letter to the Editor, while another consisted of a comparative trial of three techniques (ST, PDT and the translaryngeal procedure), primarily designed to assess the effects of the procedures upon intracranial pressure, cerebral perfusion pressure, and cerebral oxygen extraction. The authors point to the need for randomized comparative studies.
Given the equivalence among the different modalities, it is difficult to recommend a concrete technique as being better than the rest. As a result, the choice is conditioned more by professional preferences than by objective criteria.
Safety methodsFibrobronchoscopy is the most widely used safety method, though its application as a routine coadjuvant technique is heterogeneous. In effect, while in Spain fibrobronchoscopy is reportedly used in 16% of the ICUs,10 its application in other countries in our setting varies between 36%13 and 98%.15 The routine use of fibrobronchoscopy has been the subject of controversy, since the endoscopic guide produces a rise in airway pressure, hypoventilation and an increase in intracranial pressure – a situation that contraindicates its utilization in patients with acute neurological damage. Moreover, fibrobronchoscopy increases the cost of the procedure – causing some authors to consider its use only in cases with anatomical difficulties or in the context of learning curves.57 Nevertheless, the technique is simple and is recommended by some guides66 in the absence of contraindications, with a view to preventing serious complications such as false passage or damage to the posterior tracheal wall.
Capnography is useful for confirming the intratracheal location of the needle at the time of puncture. Mallick et al.67 have compared capnography with fibrobronchoscopy in 55 patients subjected to PT using the CBR technique. Twenty-nine patients were randomized to endoscopic control and 26 to capnographic control. The authors found capnography to be comparable to bronchoscopy in confirming the location of the needle in the tracheal lumen, and concluded that it may be an alternative to endoscopic guidance when the latter cannot be used or is contraindicated. The disadvantage of capnography is the lack of direct visualization of the precise position of the needle and metal guide within the trachea.
Cervical ultrasound can be useful for locating aberrant vascular structures that may cause bleeding. Kollig et al.68 performed PDT in 72 patients, initially using cervical ultrasound, followed by bronchoscopy. Based on the ultrasound findings, the puncture site had to be modified in 24% of the cases. There were no cases of damage to the posterior tracheal wall or bleeding. In this respect, ultrasound is a noninvasive procedure and may prove useful in selected patients.
Timing of tracheostomy in the ventilated patientThe optimum timing of tracheostomy in the ventilated patient remains the subject of debate. The difficulty lies in defining prolonged mechanical ventilation and predicting which patients are going to need it.
The comparative studies of early versus delayed tracheostomy have been unable to draw firm conclusions. There has been heterogeneity in defining the term prolonged mechanical ventilation, and difficulty in defining which patients are candidates for such ventilation, as well as heterogeneity in the type of patients included, randomization defects, and consequently heterogeneity of the results obtained. Since 1984, a total of 8 randomized prospective studies have been published69–76 (Table 5). Two of them71,72 found no advantages with early tracheostomy versus the delayed technique. One of these studies71 reported important difficulties in performing randomization, while the other72 was carried out in critical burn patients. The results of the three most recent studies are contradictory. While Rumbak et al.74 found early tracheostomy (within the first 48h of mechanical ventilation) to involve a shorter duration of mechanical ventilation, a shorter stay in the ICU, and lesser pneumonia and mortality, Blot et al.75 observed no differences in terms of mortality, pneumonia, days without mechanical ventilation or stay in the ICU between the patients subjected to tracheostomy in the first four days (early) versus those in which the technique was carried out after more than 7 days (delayed). In the latest and also the largest randomized prospective trial, designed to assess the incidence of ventilation associated pneumonia among patients subjected to early (6–8 days) or delayed tracheostomy (13–15 days), Terragni et al.76 observed no differences between the two groups.
Results of randomized prospective studies that have compared early versus delayed tracheostomy.
| Author | Type of patients | Number of patients | Timing of tracheostomy | Results |
| Dunham and LaMonica 69 | Trauma | 74 | Early: 3–4 daysLate: >14 days | Without differences in laryngotracheal disease |
| Rodriguez et al.70 | Trauma | 106 | Early: ≤7 daysLate: >7 days | Shorter duration of MV, stay in ICU, in hospital and even pneumonia if tracheostomy is performed before 3 days |
| Sugerman et al.71 | Trauma/non-trauma | 157 (potential) | 1st randomization: 3–5 days2nd randomization: 10–14 days | Without differences in duration of stay (ICU and in hospital), frequency of pneumonia and death |
| Saffle et al.72 | Burns | 44 | Early: next day availableLate: 14 daysa | Without differences in ventilation support, duration of stay, incidence of pneumonia or survival |
| Bouderka et al.73 | TBI | 62 | Early: 5 daysLate: prolonged intubation | Shorter duration of MV (for the early tracheostomy group) |
| Rumbak et al.74 | Clinical | 120 | Early: 2 daysLate: 14–16 days | Shorter duration of MV, stay in ICU, lesser pneumonia and mortality (for the early tracheostomy group) |
| Blot et al.75 | Polyvalent | 123 | Early: 4 daysLate: > 7 days | Without differences in mortality, pneumonia, days without MV, stay in ICU |
| Terragni et al.76 | Polyvalent without pneumonia | 600 | Early: 6–8 daysLate: 13–15 days | Without differences in incidence of VAP |
VAP, ventilator associated pneumonia; TBI, traumatic brain injury; ICU, Intensive Care Unit; MV, mechanical ventilation.
Three meta-analyses have addressed this issue. The study by Maziak et al.77 included two retrospective studies and three randomized trials with a total of 396 trauma patients with neutropenia and acute respiratory failure. The results do not suggest that the timing of tracheostomy influences the duration of mechanical ventilation or laryngeal damage. The limitations result from the heterogeneity of the included studies, heterogeneity in timing, a lack of information on how randomization was carried out, defective randomizations, and the inclusion of studies predating the PT era. In their meta-analysis, Griffiths et al.78 included 5 randomized studies comprising 406 clinical, surgical, trauma and burn patients. The timing of early tracheostomy was 0–7 days after the start of ventilation or admission to the ICU. The authors concluded that early tracheostomy results in a lesser duration of mechanical ventilation and a shorter stay in the ICU, but they recorded no differences in terms of pneumonia or mortality. Dunham and Ransom79 in turn included trauma patients in a meta-analysis comprising four retrospective studies and 5 randomized trials. The results showed no influence of early tracheostomy upon the development of pneumonia or patient mortality. Here again, the heterogeneity of the included studies did not allow the drawing of firm conclusions.
The literature suggests that early tracheostomy affords no advantages in terms of ventilation associated pneumonia or mortality, though it seems reasonable to use the technique in patients who are likely to require prolonged mechanical ventilation, in view of its benefits compared with intubation in terms of well-being, stay in the ICU and time on mechanical ventilation.
The term prolonged mechanical ventilation is characterized by important variability, and its definition is conditioned by the setting in which it is used. In our proposal of a prolonged ventilation probability model,80 we established a period of 7 days, on the grounds that this is the time limit for the possible appearance of laryngeal damage secondary to endotracheal intubation.3 Other studies have aimed to identify groups of patients with a high probability of requiring prolonged mechanical ventilation in both selected populations81–83 and in the general population.84 All of them have limitations, and no validated model is available. Therefore, considering the lack of tools that could help in the decision-making process, the timing of PT should be established on an individualized basis.
ConclusionsTracheostomy is one of the most common techniques in the ICU, and PT is a widespread practice in our setting. The popularity of the technique is based on its safety, easy execution, and the fact that it can be performed at the patient bedside. Fibrobronchoscopy has gained acceptance and is now recommended as a safety technique. Although it is difficult to define the incidence of perioperative complications (which should be analyzed for each individual PT modality), it can be regarded as no greater than that associated with ST. Nevertheless, the incidence of late complications has been little studied to date, and surveys involving larger patient samples are therefore needed to clarify this aspect. The contraindications of PT have become relativized as confidence with the technique has increased, though it must be taken into account that children, neck injuries and infection of the surgical zone remain absolute contraindications. The optimum timing of tracheostomy in the ventilated patient remains the subject of debate. The results of randomized studies contrasting early versus delayed tracheostomy are heterogeneous. Consequently, it can only be affirmed that the timing of PT should be established on an individualized basis.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Añón JM, Araujo JB, Escuela MP, González-Higueras E, por el Grupo de Trabajo de Insuficiencia Respiratoria Aguda de la SEMICYUC. Traqueotomía percutánea en el paciente ventilado. Med Intensiva. 2014;38:181–193