Plasmapheresis is the selective and automated removal of plasma. When plasma is removed and replaced by another fluid for therapeutic purposes, the procedure is referred to as therapeutic plasmapheresis or therapeutic plasma exchange (TPE).
This extracorporeal filtration process eliminates pathogenic components (immunoglobulins, auto-antibodies, immune complexes, cryoglobulins, lipoproteins, protein-bound substances and endotoxins) related to many autoimmune or non-autoimmune disorders (familial hypercholesterolemia) or acute processes in which altered substances needs to be replaced by normal components (thrombotic thrombocytopenic purpura, thyroid storm).
The fluid that replaces the plasma must possess the physiological functions of the latter, and be both isovolumetric and iso-oncotic. The most commonly used fluids are fresh frozen plasma (FFP) and albumin solutions. Both can cause complications,1,2 such as the loss of plasma proteins and coagulation factors in the case of albumin, or allergic reactions, the risk of viral transmission, citrate reactions and hypocalcemia in the case of FFP.
Plasmapheresis classically has been performed by centrifugation (c-TPE),3,4 though the development of membrane-based techniques (m-TPE) (involving convection through a filter with highly permeable membranes) offers important advantages: simplicity, accessibility, lower cost, no loss of cellular components, and no need for anticoagulation in many cases.5,6 The added fact that m-TPE can be performed using common dialysis systems or continuous renal replacement therapy (CRRT) techniques explains its increasing use in recent years and its incorporation into the Intensive Care Unit (ICU).7–10
In order to evaluate the adoption of this technique by the ICUs of the Community of Madrid (Spain), in October 2021 we sent a survey to the respective Heads of the different Units, with the collaboration of the Society of Intensive Care Medicine of Madrid (SOMIAMA) (Annex 1), addressing three main aspects: (1) the use of TPE in and outside the ICU, and who performs the technique; (2) the logistics (resources and organization) for TPE in the ICU; and (3) the treated patients and their origin.
The survey was answered by a total of 37 ICUs (Annex 2): 24 belonging to public hospitals (out of a total of 26; 92.3%) and 13 to private hospitals (out of a total of 29; 44.8%). Table 1 shows the characteristics of the participating hospitals/ICUs.
Characteristics of the participating hospitals and Intensive Care Units.
| No. hospital beds | Hospital complexity | No. ICU beds | Is plasmapheresis performed at your hospital (out of the ICU)? | Department performing plasmapheresis out of the ICU | Is plasmapheresis performed in your ICU? | Department performing plasmapheresis in the ICU |
|---|---|---|---|---|---|---|
| Public hospitals | ||||||
| 1700 | High | 40 | Yes | Nephrology | Yes | ICU, Nephrology |
| 1200 | High | 41 | Yes | Hematology | Yes | ICU |
| 1200 | High | 38 | Yes | Nephrology | Yes | ICU, Nephrology, Hematology |
| 900 | High | 24 | Yes | Hematology | Yes | Nephrology, Hematology |
| 700 | High | 38 | Yes | Hematology | Yes | Hematology |
| 660 | High | 18 | Yes | Hematology | Yes | Hematology |
| 610 | High | 22 | Yes | Hematology | Yes | Hematology |
| 495 | High | 22 | Yes | Hematology | Yes | Hematology |
| 504 | Medium | 18 | Yes | Nephrology | Yes | ICU, Nephrology |
| 450 | Medium | 24 | Yes | Hematology | Yes | Nephrology, Hematology |
| 420 | Medium | 12 | Yes | Hematology | Yes | Hematology |
| 420 | Medium | 16 | Yes | Nephrology | Yes | ICU |
| 400 | Medium | 16 | Yes | Hematology | No | |
| 358 | Medium | 12 | No | Yes | ICU | |
| 350 | Medium | 8 | Yes | Nephrology | No | |
| 325 | Medium | 18 | Yes | Nephrology | Yes | Nephrology |
| 300 | Medium | 12 | No | Yes | ICU | |
| 300 | Medium | 14 | Yes | Nephrology | Yes | Nephrology |
| 250 | Medium | 16 | Yes | Nephrology | Yes | ICU, Nephrology |
| 325 | Low | 16 | No | No | ||
| 200 | Low | 12 | No | No | ||
| 130 | Low | 11 | Yes | Nephrology | Yes | ICU, Nephrology |
| 100 | Low | 8 | No | Yes | ICU | |
| 90 | Low | 4 | No | No | ||
| Private hospitals | ||||||
| 250 | 14 | Yes | Hematology | Yes | Hematology | |
| 190 | 16 | No | No | |||
| 180 | 6 | No | No | |||
| 180 | 12 | Yes | Hematology | Yes | ICU | |
| 170 | 16 | No | No | |||
| 120 | 17 | No | No | |||
| 120 | 12 | No | Yes | ICU, Hematology | ||
| 100 | 9 | No | Yes | ICU | ||
| 90 | 12 | Yes | Hematology | Yes | ICU | |
| 86 | 9 | No | No | |||
| 80 | 12 | No | Yes | ICU | ||
| 60 | 7 | No | Yes | ICU | ||
| 20 | 3 | No | No | |||
In 9 hospitals (24.3%) TPE was not performed either in or out of the ICU: three public centers (all 3 of low complexity) and 6 private centers (all with <200 beds).
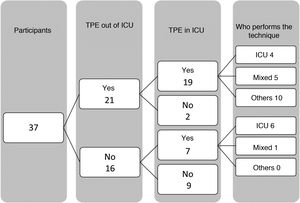
Twenty-one hospitals (56.7%) performed “central” TPE (i.e., out of the ICU) (18 public centers; 77% and 3 private centers; 23%), and the procedure was carried out in 12 cases (57.1%) by Hematology and in 9 cases (42.9%) by Nephrology. Of the hospitals without “central” TPE (16 centers; 43.2%), the technique was performed in the ICU of 7 of them (43.75%).
On the other hand, 70.3% (26) of the hospitals performed plasmapheresis within the ICU, though the technique was only carried out by ICU professionals in 10 cases (38.5%) and in combination with other professionals (hematologists or nephrologists) in another 6 Units (24%). In other words, in 10 of the ICUs (38.5%) where plasmapheresis was carried out, intensivists did not participate in the technique (Fig. 1).
Of the 26 ICUs that performed TPE, the technique was only used in ICU patients in 7 Units (26.9%), in ICU patients and patients admitted to the hospital ward in 14 (53.8%), only in hospital ward patients in one Unit (3.8%), and in hospital ward, ICU and ambulatory patients in four ICUs (15.4%).
In all the ICUs in which TPE was performed by ICU professionals (20 Units), use was made of m-TPE with CRRT systems; one ICU could not specify the monitor used, and in the 5 ICUs in which TPE was performed by Hematology, use was made of c-TPE with machines belonging to the Hematology Department.
With regard to availability for performing the technique, 14 ICUs (53.8%) were able to carry it out at any time during 365 days a year; only in the morning but on any day of the year in four ICUs (15.4%); only on working days at any time in two (7.7%); and only in the morning on working days in 6 ICUs (23%).
The professionals able to prescribe and perform the procedure represented only a limited group within the overall staff in 7 Units (26.9%), while in the remaining 19 (73%) TPE could be performed by any physician or nurse. Of note is the fact that in 8 ICUs with such availability, the technique was not performed by intensivists but by hematologists or nephrologists.
The mean number of patients treated in the ICU was 5.25/year, with an average of 4.3 sessions per patient.
The usefulness of plasmapheresis is evident. Most of the patients are not in a critical condition and do not have to be admitted to the ICU to perform the technique. Most high and medium complexity Spanish hospitals have Departments that carry out the procedure (Hematology, Nephrology). When a critical patient requires this kind of treatment, these are the Departments generally in charge of performing the technique, and moreover constitute reference Departments for those hospitals that do not have plasmapheresis.
In the case of hospitals without “central” TPE, the possibility of performing plasmapheresis in the ICU has clear advantages, since timely and optimum treatment can be provided as needed, without requiring patient transfer (with its inherent disorders and risks). On the other hand, coverage can be provided for non-critical patients pertaining to other specialties, admitted to the hospital ward or on an ambulatory basis.
The results of the present survey show that in most hospitals with “central” plasmapheresis (Hematology or Nephrology), TPE in the ICU is also performed by these “out-ICU” professionals - though this should not be an obstacle for application of the technique by professionals of the ICU.
Less than half of the hospitals that do not have “central” TPE perform the technique in the ICU, and in all cases the professionals of the ICU are those that carry out the procedure. In other words, over one-half of these hospitals must transfer the patients to undergo plasmapheresis.
In a large proportion of the participating ICUs the technique is widely available in terms of both time and trained professionals for performing TPE. This guarantees that any patient requiring the technique will have it available at all times.
The survey also evidences the availability of the ICUs for performing TPE in any patient (not only critical cases). Of the ICUs that perform TPE, almost 70% can also provide this service for hospitalized non-critical patients, though only 15% offer the technique for non-hospitalized (ambulatory) patients.
The ICU may be a good place to perform TPE. It possesses the necessary technical means, with optimum monitoring capacity and staff trained to perform the technique. This possibility enhances hospital performance and the services offered by the Department of Intensive Care Medicine. In addition, possibilities are opened for collaboration with other Departments, thereby expanding the scope of intensive care medicine.
Conflict of interestThe authors of the study entitled: “Plasmapheresis in the Intensive Care Units of the Community of Madrid (Spain)” declare that they have no conflicts of interest. They have no ties, activities or interests related to the contents of the manuscript (there are no profit or non-profit relations with third parties that may be affected by the contents of the article).