When hospitalized patients with pulmonary arterial hypertension (PAH) often fare worse compared to patients with other conditions. It is for this reason that the current COVID-19 pandemic has posed a specific challenge for these patients.1
Experts from 32 centers specialized in the management of PAH from the United States gave their answers to an electronic survey sent by the Pulmonary Hypertension Association and only reported on 13 cases treated of which only 1 patient did.2 These results, based on data collected at the beginning of the pandemic in the United States, should be interpreted with caution. Also, the results of this survey may be subject to response bias because it is still unclear how many centers responded to the survey or how many patients with PAH were included to find 13 patients who tested positive for COVID-19. However, in Italy it was also striking to see that chronic obstructive pulmonary disorder (COPD) was not among the main comorbidities of the patients who died.3 Also, a study on the characteristics of 1591 patients admitted to an intensive care unit in Lombardy, Italy found that COPD amounted for just 4% of the main comorbidies.4
In light of these surprising results, Horn et al.2 questioned several things, among them, if PAH and its preexisting pulmonary vasculopathy could be protecting these high-risk patients, whether an impaired pulmonary endothelium could be the cause of a significant impairment of the inflammatory response, and if hypoxemia played a role in viral replication.
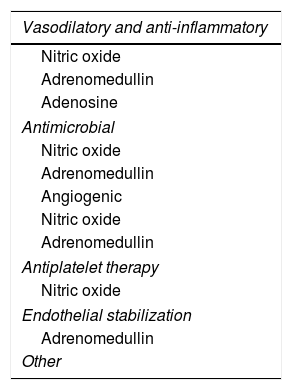
Two years ago I published a paper in Medicina Intensiva where I was trying to associate altitude-induced hypoxia with hypoxia in the critically-ill patient.5 In that paper I mentioned that hypoxia-inducible factor (HIF-1) that can be found in almost every tissue of the human body degrades due to hydroxylation under normoxic conditions. However, it does not degrade with hypoxia. Instead, it grows exponentially activating numerous cytoprotective genes and facilitating a greater oxygen supply to the tissues and a lower use of such oxygen. Nitric oxide (NO), adrenomedullin, and adenosine (Table 1) are among the gene products regulated by HIF-1 thanks to their properties and physiological effects. It is said that people from Tibet who are used to living at high altitudes had higher NO levels when compared to people who live in lowlands. Actually, mountain men who live at altitudes above 5000 m for over a month have high HIF-1 levels during their stay and, consequently, activate the genes that depend on this factor. On the other hand, HIF-1 plays a significant role in oxygen homeostasis, not only in acclimation to altitude hypoxia, but also in the hypoxemia/inflammation molecular response that is prevalent in sepsis. The reduction of its levels is directly associated with the severity of sepsis.6
Main effects and actions of nitric oxide, adrenomedullin, and adenosine.
| Vasodilatory and anti-inflammatory |
|---|
| Nitric oxide |
| Adrenomedullin |
| Adenosine |
| Antimicrobial |
| Nitric oxide |
| Adrenomedullin |
| Angiogenic |
| Nitric oxide |
| Adrenomedullin |
| Antiplatelet therapy |
| Nitric oxide |
| Endothelial stabilization |
| Adrenomedullin |
| Other |
Mitochondrial biogenesis and improved production of ATP (nitric oxide).
Positive influence in conditions that start with hypoxia: they favor cellular tolerance to oxidative stress and hypoxic lesions (adrenomedullin).
Protector against pneumonia while on mechanical ventilation (adrenomedullin).
«Guarding Angel» against cellular damage because it rises its levels in situations of ischemia/acute hypoxia (adenosine).
In PAH there is pulmonary arterial vasoconstriction and depending on its etiology, hypoxemia of variable tolerance that can be severe. Endothelial dysfunction and vascular remodeling are 2 significant processes that take place in the development of PAH. It has been suggested that endothelial dysfunction with its thrombotic consequences seen in COVID-19 hyperinflammatory phase is not as florid in patients with PAH since they already have preexisting endothelial dysfunction. We should not forget that we are dealing with a chronic state of hypoxia and, therefore, the physiological effects, among other cytoprotective and antiplatelet effects of NO, adrenomedullin, and adenosine as shown on Table 1.
Due to their hypoxemia, patients with PAH often develop polycythemia. Clinical research has been focusing on NO derived from the endothelium mostly. A recent study showed that NO is also a derivative of red blood cells, which opens important fields of research for new therapeutic applications that counterbalance hypoxia-induced tissue damage. This NO derived from red blood cells regulates and maintains the deformity of red blood cells in cases of severe hypoxia and triggers the release of oxygen.7 Whether polycythemia has certain prophylactic properties should be studied.
It has been hypothesized that, when COVID-19 kicks in, not every patient develops acute respiratory distress syndrome (ARDS). This has been attributed to a possible loss of hypoxic vasoconstriction and an impaired regulation of pulmonary blood flow.8 It is possible that in PAH this regulation barely changes since there is a significant prior vasoconstriction associated that exerts some protective effect on this loss of regulation.
The last question here would be whether hypoxemia can play a role in viral replication. Two papers already published may have the answer to this question. In an animal model Thompson et al.9 studied the association between hypoxia and bacterial infections, which is often coexistent. The murine model showed that during the acute infection phase, both local and systemic, results were catastrophic due to an exaggerate response triggered by the activation of neutrophils associated with HIF-1. However, the most striking finding was that a state of chronic hypoxia achieved through hypoxic preconditioning before the infection protects against the higher morbidity and mortality rates seen in acute hypoxia because it prevents this exaggerate leukocyte response mediated by HIF-1.
On the other hand, in 2005, Akerström et al.10 showed that NO, a molecule activated by HIF-1, inhibits the cycle of replication of coronavirus in ARDS induced by SARS-CoV. However, to this day, there are no studies on SARS-CoV-2 or COVID-19, but it is expected that the role of NO on both coronaviruses will be the same.
ConclusionsWe live in a time when express publications with poor or none scientific evidence can be misleading and not bring any scientific value. Our intent was to avoid being controversial. Instead, we decided to use the existing medical literature to try to answer to the questions posed by Horn et al.2 on the low incidence and mortality rate of patients with PAH during the current COVID-19 pandemic. Also, we wanted to show our recognition towards these clinical trials on the incidence and progression of PAH during the COVID-19 pandemic. Only then we’ll know for sure whether the low incidence and mortality reported was another speculation.
FundingThe author did not receive any funding whatsoever.
Conflicts of interestNone reported.
Please cite this article as: Avellanas Chavala ML. Hipertensión arterial pulmonar y COVID-19. Med Intensiva. 2020;155:577–579.