We, intensivists, lead critically ill patient care through a model that has proven efficient and improved health results.1 This model requires a specifically organized staff under proper labor conditions.2,3 Shift work with calls in the critical care setting requires management focused on taking care of the health professionals involved.4,5 Inappropriate labor conditions are associated with higher chances of occupational accidents in itinere, chronic diseases, and burnout syndrome.6 Despite its importance, the attention paid in our organizations is scarce. Experience in other countries warn us on the importance of these aspects and comprehensive plans have been envisioned on this regard.7,8 The SEMICYUC Youth working group proposed conducting a survey to get to know the actual labor situation of intensivists within their first few years of practice. The scientific approval from SEMICYUC was obtained for this purpose. Approval from clinical research ethics committee was not deemed necessary given the voluntary and anonymous nature of the survey. All members acting as specialists within their first 10 years of practice were asked to participate through an e-mail sent to them. The period of the survey spanned from December 2020 through September 2021 and recruitment was increased during the pandemic. The survey is available for consultation on the supplementary data (Appendix B; supplementary data 1). Data obtained are shown based on a descriptive statistical analysis with number (percentage) or median (interquartile range [IQR]). Results were grouped into 3 different categories: 1) Overall characteristics of the population and labor conditions; 2) Opportunities at the working station and talent retention; 3) Conciliation of personal, family and working life and attention to the health professional. Since the COVID-19 pandemic has caused changes to the respondents’ working situation, a distinction was made between the situation prior to the pandemic and the situation afterwards.
A total of 100 answers were submitted. The number of intensivists with 10 or less years of experience when the survey was conducted was 1050 while the rate of response was 9.5%. A total of 74% of the patients were women with a mean age of 33 (31-36) years. A total of 65% of respondents had finished their residencies over the past 5 years (Appendix B; supplementary data 2). The most highly represented autonomous communities were Catalonia (14%), and the Community of Madrid (13%) (Appendix B; supplementary data 2). The most common type of contract was temporary (79.3%) followed by indefinite (18.5%). A total of 47% worked for the Spanish National Health System (NHS) alone while 46% also worked for the private sector and the NHS too. Only 4% worked for the private sector alone. A total of 82% conducted their clinical activity at the intensive care setting while the rest shared this activity with other settings like the ER (both in- and out-of-hospital). The median of employees was 2 [1–3]. Respondents did a total of 6 calls/month [5–7] and up to 7 [6–8] during the pandemic. We should mention that 18.8% of respondents did a total of > 8 calls routinely (up to 39% during the pandemic).
Regarding working opportunities, 54% said they were master’s degree holders while 12% claimed were studying a master’s degree while the survey was being conducted. Only 6% were PhD holders while 16% said they were currently studying to become PhDs. A total of 26% stated that they participated in some kind of funded research project A total of 43.8% considered that their participation in training and research activities was not encouraged. A total of 59% stated that they had had second thoughts about changing their medical specialty recently while 61% were already thinking of working in other country.
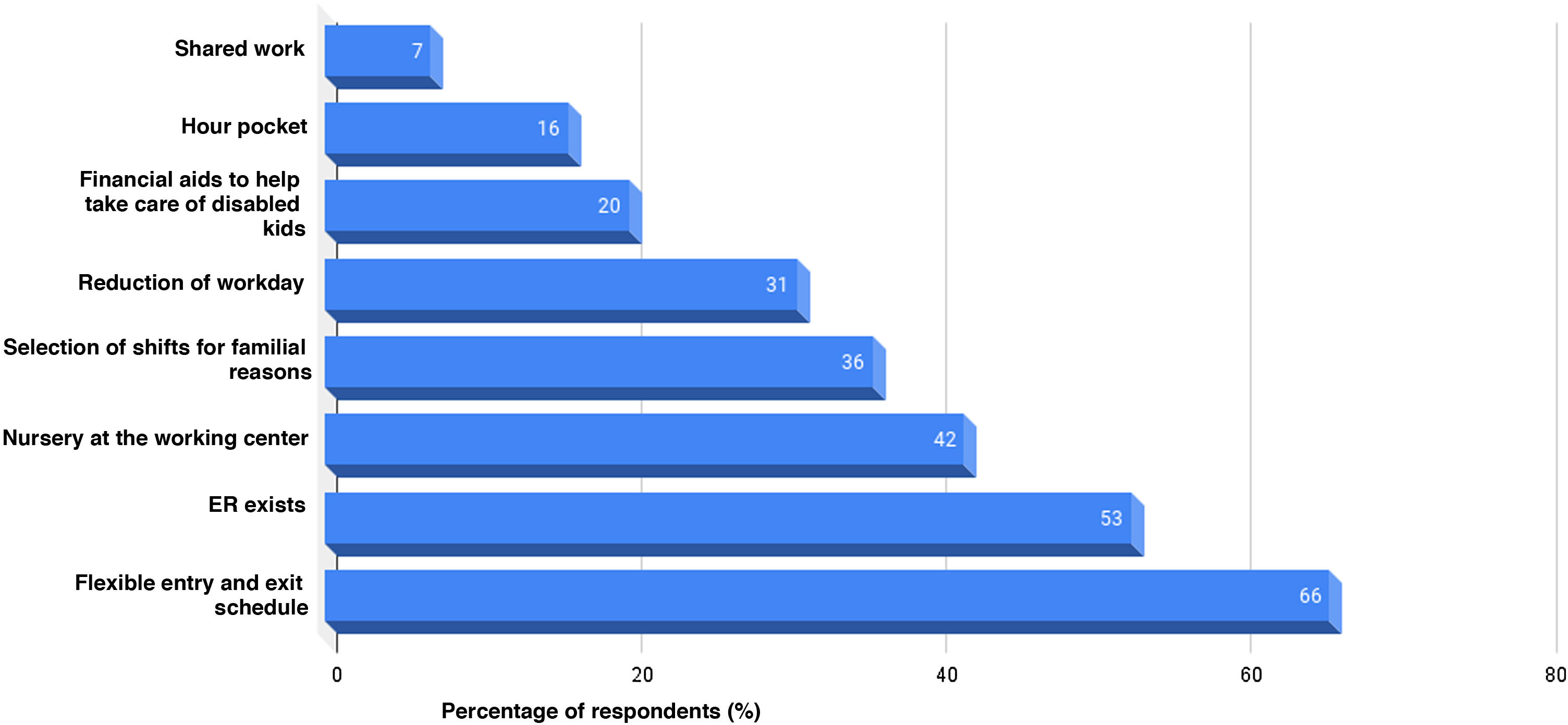
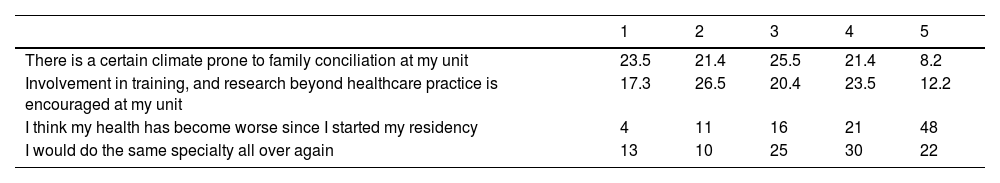
Finally, the possibilities of conciliation of personal, family and working life were studied. A total of 34% of respondents were in charge of family members. When asked on how difficult it was to match their professional and personal lives, 57% responded “difficult” or “very difficult”. Respondents were asked to assess different statements on care and conciliation (Table 1). We should mention that 44% did not identify a climate prone to conciliation at their unit while half of them thought their health had become worse since the beginning of their residency. Among the measures proposed to improve the working conditions (Fig. 1), the ones most widely accepted were the presence of a flexible schedule (66%), and the existence of hour pockets for emergencies associated with family members and care (53%).
Conciliation of personal, family and working life and attention of health professionals.a
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| There is a certain climate prone to family conciliation at my unit | 23.5 | 21.4 | 25.5 | 21.4 | 8.2 |
| Involvement in training, and research beyond healthcare practice is encouraged at my unit | 17.3 | 26.5 | 20.4 | 23.5 | 12.2 |
| I think my health has become worse since I started my residency | 4 | 11 | 16 | 21 | 48 |
| I would do the same specialty all over again | 13 | 10 | 25 | 30 | 22 |
This survey is the starting point to analyze the working situation of our medical specialty. Results show high levels of transitoriness (above half of the sample studied). Also, the lack of strategies aimed at retaining and promoting talent and conciliation issues were evident in the answers given. Data require raising awareness to make sure that health professionals in charge of critically ill patients have the necessary life and working conditions to do their job with quality and safely.2–4 The impact this situation can have can be described in 3 different levels. In the first place, impact on the quality of care with several studies associating the health professionals’ wellbeing with quality and safety of care.6,7,9 Secondly, on the health professionals’ wellbeing since working conditions have been associated with more diseases, labor absenteeism, rotation, and higher costs for the entire healthcare system. Finally, impact on the very future of our medical specialty.3,8 In this sense, both the strategic plan of our society and the international studies on this regard include some working lines to improve this situation.1,4,6 Results should be assessed with caution given the scarcity of data. Results come from an age range of all the respondent specialists, yet the rate of response was scarce despite the interest associated with the topic at stake. In any case, only a generation of intensivists with proper working stability, motivated, and involved with different organizations can be the foundation upon which the future of our medical specialty can be built.
FundingNone whatsoever.