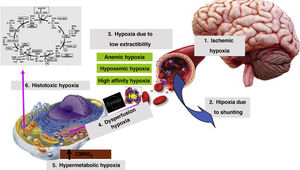
Traditionally, in the management of patients with severe traumatic brain injury (STBI), recommendations focus on keeping intracranial pressure under control. It is surprising to see that there are no specific indications on the management of anemia.1 From the pathophysiological standpoint, disregarding the levels of hemoglobin (Hb) probably means reaching proper levels of cerebral perfusion pressure, but with a poor quality in tissue oxygenation (Fig. 1). It is unquestionable that, in this context, our clinical practice guidelines should follow the European recommendations on “Patient Blood Management” to minimize blood losses, optimize homeostasis and, therefore, stop, in a multidisciplinary way, the patient from becoming anemic by avoiding unnecessary transfusions.2
However, the main problem we face when assessing the medical literature available on STBIs is the heterogeneity of the studies published that often mix patients with moderate TBIs with authors that use different transfusion thresholds based on the hematocrit or on the levels of hemoglobin (Hb). Also, we should mention that most observational studies published to this date analyze the impact of anemia or the effects of red blood cell transfusion on the prognosis of traumatic brain injury.3–7
Specifically, certain working groups state that in TBIs, anemia is associated with higher rates of complications and mortality.3,4 Other studies, however, propose a different hypothesis, claiming that Hb levels > 9 g/dL are associated with a better functional prognosis.5
Despite of this, we should mention that the solution is not transfusing this subpopulation of neurocritical patients systematically. As a matter of fact, some authors say that the transfusion of red blood cell concentrates is associated with a poor long-term prognosis.6–8 In this sense, Desjardins et al. working group conducted a systematic review on this matter, but could not draw any definitive conclusions because the study was underpowered due to the lack of homogeneity in the protocols analyzed.9 However, they claim that blood transfusion was associated with a worse functional prognosis during the management of both moderate and severe TBIs. Nonetheless, a recent retrospective trial identified that a restrictive transfusion approach can be a safe and cost-effective practice.10
Despite the interest associated with transfusion strategies during the management of STBI, the number of clinical trials available to this date is still scarce. We should mention the post-hoc analysis conducted by McIntyre et al. back in 2006. In this study, the authors found no morbidity or mortality differences in the transfusion restrictive strategy (7 g/dL to 9 g/dL) compared to the more liberal one (Hb, 10 g/dL to 12 g/dl).11 However, in spite of design limitations, it is striking to see that the recruitment of patients did not include each patients’ specific level of consciousness according to the Glasgow Coma Score (GCS). Also, when the characteristics of the population were analyzed, there were barely any significant personal health records between both arms. Afterwards, the clinical trial conducted by Robertson et al. was published. This trial was approached from 2 different perspectives in terms of both the transfusion threshold and the possible utility of erithropoietin.12 Despite the early expectations this trial generated, we can identify several limiting factors. In the first place, the patients underwent a change of protocol due to the administration of erythropoietin, which extended the duration of the trial for another 6 years. Secondly, the patients of each group had Hb levels above the target values. Thirdly, the sample size per group was relatively small. In their results, the authors did not find any differences in terms of survival or prognosis. We should mention that the liberal transfusion group developed more infections, thromboembolic events, and respiratory distress syndrome. The TRAHT pilot study has recently been published. It reveals that the clinical design of the study is feasible. It also anticipates that patients included in the liberal transfusion group had better recoveries and lower mortality rates. The authors state that optimizing brain oxygenation can be a key factor in their results.13 In conclusion, we will have to wait for the definitive results not only from this clinical trial but also from the TRAIN and HEMOTION trials before having more evidence available on this regard. However, we should not forget that clinical trials are always based on ideal scenarios since complex patients with comorbidities and previous treatments are not usually recruited in these studies.
At the same time, it is obvious that our management of patients with STBI who may require transfusions cannot be based on a simple figure appearing on the lab result record sheet, especially if there are specialized units with multimodal neuromonitoring systems available capable of providing reliable information from different pathophysiological angles on the actual situation of the brain. In this sense, we found several trials that analyzed the capacity of PtiO2 to recognize situations of anemia and brain hypoxia that also proved the effects of transfusion on brain oxygenation.14,15 Also based on the study conducted by Robertson et al. we found a subanalysis oriented to the information obtained from the neuromonitoring of patients with STBI.12,16 The authors identified that the restrictive strategy group developed more episodes of brain hypoxia when the sensor was placed in healthy areas of the brain. However, no differences were found in the mortality rate described between the restrictive strategy group and the liberal strategy group. Afterwards, Leal-Noval et al. working group conducted an interesting clinical trial in which the transfusion threshold was guided by the Hb levels and the rSO2. The authors proved that there was a lower need for transfusions when both triggers were used without identifying any differences between both groups.17
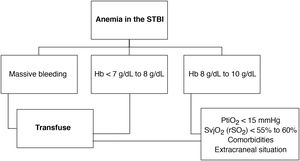
To this point, we can say that there is not a single clear piece of evidence that tells us when we should transfuse patients with STBI with Hb levels between 8 g/dL and 10 g/dL. The decision-making process to this point is still controversial, and open to discussion. It is obvious that more information is required when it comes to establishing the transfusion indication. In these cases, and taking the aforementioned considerations into account our opinion is that Fig. 2 is a good guideline on how to proceed on this regard. This way we would be profiting from all the information obtained through advanced neuromonitoring when facing this transfusion uncertainty, and once other causes of tissue hypoxia have been ruled out (Fig. 1). Still, we know that not all centers can systematically monitor ICP, PtiO2, and rSO2.16,18 Finally, we should be taking into account the patient’s past medical history, as well as the presence of other bleeding traumatic injuries associated with STBI.
In conclusion, we should mention the need to widen our knowledge in this area that deals with the management of patients who sustain STBIs to establish transfusion indications through objective, safe, and efficient criteria.
Conflicts of interestNone reported
Please cite this article as: Egea-Guerrero JJ, García-Sáez I, Quintana-Díaz M. Trigger transfusional en el paciente con traumatismo cráneo-encefálico grave. Med Intensiva. 2022;46:157–160.