Clinical examination is essential at the intensive care unit (ICU) setting, above all in the assessment of patients with primary neurological disorders, as well as in the detection of secondary neurological disorders. It is recommended that all critically ill patients should undergo a routine neurological examination being pupillary examination (symmetry and pupillary reactivity) one of the most significant components from the prognostic perspective.
Traditional pupillary examination includes the size, symmetry, and pupillary light reflex (PLR) to qualitative light. This examination is of a visual and qualitative nature and is often based on the use of manual flashlights, which is prone to common mistakes of detection and interpretation,1 which exposes the lack of a standard examination strategy, which could eventually lead to diagnostic delays or the performance of unnecessary procedures with adverse clinical outcomes.
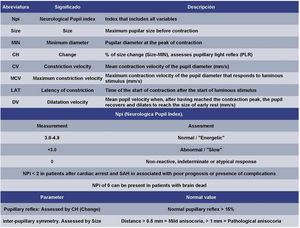
Brief description of the techniqueOver the last few years, a new tool for neurological assessment has joined the therapeutic armamentarium: automated quantitative optical pupillometry (Fig. 1). This examination is conducted with a pupilometer. This device allows precise and reliable non-invasive quantitative examinations that measure different pupillary parameters (Fig. 2) by avoiding the mistakes and biases associated with standard qualitative examinations. Currently, two devices are available at the market: Neuroptics® NPi-200, and Neurolight Algiscan®. Both devices share similar features although depending on the device there are other additional variables that can be measured in one of these devices only like the so-called Neurologic Pupil Index in NPi-200, which is based on a mathematical algorithm patented by the manufacturer.2 Although there are different scenarios, and possible potential applications regarding the ICU setting,2 we’ll now focus on the 3 scenarios of neurocritical condition where the application of this technique is backed by the largest evidence compiled to this date or ongoing studies like the prognostic assessment of patients after cardiac arrest (post-CA), the detection of intracranial hypertension, and the detection and diagnosis of secondary brain damage.
Quantitative pupillometry. A) NPi-200 pupillometer. B) Pupillometry parameters, and measurments. C) Videorecording or pupillary examination. D) Pupillometry of a patient after cardiac arrest within the first 24 hours. E) Pupillometry with NPi of 0 in the same patient within 48 hours after cardiac arrest who later progresses into brain dead.
One of the most studied applications in pupillometry and the one that has gained the heaviest scientific weight over the last few years is the assessment of neurological prognosis of post cardiac arrest patients. In a prospective cohort, Suys et al.3 analyzed 50 comatose patients after cardiac arrest on targeted temperature management (TTM) assessed with quantitative pupillometry and qualitative PLR whose AUC to predict poor outcomes was higher for the quantitative PLR compared to the qualitative PLR across different timeframes (day 1, 0.79 vs 0.56, P = .005; day 2, 0.81 vs 0.64, P = .006). Patients with good neurological prognosis had higher quantitative PLR values compared to patients with poor prognosis. The prognostic accuracy of quantitative PLR was similar to that of the electroencephalogram (EEG) and somatosensory evoked potentials (SEP) (AUC 0.81 vs 0.80 and 0.73, respectively, both P > .20). Solari et al.4 found similar results in their study where comatose survivors after cardiac arrest had higher quantitative PLR values and constriction velocities compared to non-survivors. After 48 h, quantitative PLR values < 13% were associated with a 100% specificity and a 0% rate of false positives.
Possibly, the most relevant study conducted to this date is the one published by Oddo et al.5 who conducted a multicenter international study of 456 patients by comparing quantitative pupillometry using the NPi and qualitative PLR. Investigators found that at any time between days 1 and 3, NPi values ≤ 2 predicted unfavorable neurological prognoses (defined by a Cerebral Performance Category [CPC] score between 3 and 5), a 100% specificity and a 32% sensitivity. The combination of an NPi ≤ 2 with bilateral absence of N-20 in SEP provided higher sensitivity (58% vs 48% compared to SEP alone) and a similar specificity (100%). Also, 56 out of the 123 patients had normal SEP and unfavorable neurological prognosis (that is, false negatives), and 15 (27%) NPi ≤ 2. Therefore, the unfavorable prognosis was predicted correctly with quantitative pupillometry alone.
Also, the utility of pupillometry in patients on VA-ECMO and patients on CPR (ECPR) has been studied. Miroz et al.6 found that using pupillometry, an abnormal NPi (< 3, at any time between 24 h to 72 h) was 100% specific to predict 90-day mortality with a 0% rate of false positives. On the other hand, an NPi = 0 at the beginning of VA-ECMO (N = 9) was 100% predictive of mortality. Also, Menozzi et al.7 assessed pupillometry in patients with similar characteristics only to find that, in the group treated with ECPR, 2 out of 9 patients with an NPi ≤ 2 at admission had good neurological prognosis (CPC score 1-2). Therefore, the decision to start ECPR support should not only be based on the assessment of pupillometry at admission.
Quantitative pupillometry to detect elevated intracranial pressureElevated intracranial pressure (ICP) can cause alterations in pupillary assessment. The first investigators to apply quantitative pupillometry in this setting were Taylor et al.8 who found that in 13 patients with midline displacement > 3 mm, elevated ICP levels > 20 mmHg for > 15 min were associated with decreased pupil constriction velocity ipsilateral to the lesion. In 5 patients with diffuse brain swelling but no midline displacement no decreased constriction velocities were found until the ICP levels exceeded 30 mmHg. A multicenter study that included 134 patients assessed using pupillometry and the NPi found no association between an abnormal NPi (< 3) and elevated mean ICP > 30 mmHg, while a normal NPi (3–5) was associated with mean ICP levels < 20 mmHg.9 In an observational study of 54 patients with severe traumatic brain injury (TBI) and monitorization of ICP and pupillometry measured every 6 hours, the tendencies of NPi across time were studied and it was found that subjects with sustained intracranial hypertension (ICH) were associated with a concomitant reduction of NPi. Also, the abnormal values of NPi were more common in patients with refractory ICH and associated with unfavorable prognosis at 6 months (Glasgow Outcome Scale [GOS] between 1 and 3).10
Regarding the utility of pupillometry in ICH we should mention that it is not only important to determine isolated abnormal values, but also changes occurred during this time. Former studies have reported changes to the NPi after the administration of osmotherapy in patients with intracranial hypertension.8 Similar findings have been made by measuring the pupil constriction velocity seeing changes to the pupil dynamics of patients with ICH associated with the administration of mannitol and implantation of external ventricular drainage, which is why quantitative pupillometry could play a certain role in the monitorization of response to the management if ICH.
Quantitative pupillometry in the detection and diagnosis of secondary brain damageGiven the high potential of pupillometry as a monitoring and neurological diagnostic tool, the possible range of uses has been widened. Taking this into consideration and using a multi-center registry, Aoun et al.11 studied 54 patients with subarachnoid hemorrhage (SAH) assessed with qualitative pupillometry every 4 h. They found a significant (P < .001) and strong (OR, 3.3930) correlation between the development of delayed cerebral ischemia (DCI) and lower NPi (<3). Seven of the 12 patients who presented with DCI had a lower NPi <3 after a normal early reading. In 5 of these patients, the reduced NPi occurred > 8 hours before presenting with neurological clinical impairment.
Currently, there is an ongoing international multicenter study (NCT04490005) analyzing the association between an abnormal pupil function, assessed using the NPi, and the long-term prognosis of patients with acute brain injuries (TBI, SAH, and intracranial bleeding).
ConclusionsQuantitative pupillometry provides fast, reliable, and precise bedside assessments of critically ill patients. Also, it has a huge potential for monitoring and early detection of brain injuries occurred at the ICU setting. Recent multicenter data tells us that the NPi has high specificity to predict unfavorable prognoses assessed using the GOS (for neurovascular conditions or TBI) or CPC scores (in patients with post-anoxic encephalopathy), when appropriate, even early in comatose patients after cardiac arrest. Therefore, we should consider adding this assessment and neurological complication detection tool to our therapeutic armamentarium to homogenize such an important assessment, increase our capacity to detect complications early, and reduce the rate of mistakes in the decision-making process, especially from the prognostic perspective of neurocritical patients.
FundingThis study received no funding from public or private entities whatsoever.
Conflicts of interestNone reported
We wish to thank Professor Dr. José Garnacho Montero for his invitation to write this manuscript.
Please cite this article as: Blandino Ortiz A, Higuera Lucas J. Utilidad de la pupilometría cuantitativa en la unidad de cuidados intensivos. Med Intensiva. 2022. https://doi.org/10.1016/j.medin.2021.12.003