The characteristics of the Units that treat neurocritical patients with cerebrovascular disease are highly variable and can influence the care which such individuals receive.1 The Neurointensive Care and Trauma Working Group of the SEMICYUC has conducted a survey on the management of neurocritical patients.2 The characteristics of the survey, the structural aspects of the centers that participated in it, and the common treatment features of all the diseases have been reported elsewhere.2 The present study analyzes the clinical aspects referred to patients with central nervous system (CNS) disorders of cerebrovascular origin (non-traumatic subarachnoid hemorrhage [SAH] and acute cerebrovascular disease [ACVD] of hemorrhagic and ischemic origin). The data obtained are reported as frequencies (percentages) or the median (interquartile range [IQR]).
Forty-one valid responses were received (response rate 22.3%). The centers that answered the survey are specified in online Supplementary material.
Subarachnoid hemorrhageA total of 28 centers (70.7%) treated patients with SAH. The median (IQR) patients/year was 33 (40). The intensivist supervised initial care in 51.7% of the centers.
The following scales were used: Hunt-Hess 93.1%, World Federation Neurological Surgeons 51.7% and Fisher 96.6%. A total of 27.6% of the centers used corticosteroids for the control of headache. In turn, 31% administered antiseizure prophylaxis (27.6% in low-grade SAH and 3.4% on a routine basis), and 41.4% performed triple H (hypertension, hypervolemia, hemodilution) therapy – in all cases using noradrenaline.
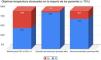
The monitoring of intracranial pressure (ICP) in patients with Glasgow Coma Scale (GCS) <9 and the aspects related to the diagnosis and management of the aneurysm are summarized in Fig. 1. Treatment of the aneurysm was preferentially endovascular. In almost all 28 of the centers that treated this disease, surgery was performed in less than 25% of the cases. A total of 89.7% had a specific management protocol, and 27.6% had participated in multicenter studies during the previous 5 years.
Acute hemorrhagic cerebrovascular diseaseA total of 37 centers (90.2%) treated patients with ACVD of hemorrhagic origin. The median (IQR) patients/year was 30 (25). The intensivist supervised initial care in 54.1% of the centers.
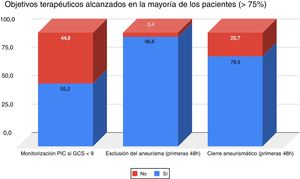
A total of 10.8% of the centers used corticosteroids to treat perilesional edema, and 32.4% administered antiseizure treatment on a routine basis. In turn, 33.3% of the centers monitored intracranial pressure in 76–100% of the patients with GCS < 9. The blood pressure targets in the acute phase, and the most frequently administered drugs used for this purpose are described in Fig. 2. A total of 40.5% had a specific management protocol, and 5.4% had participated in multicenter studies during the previous 5 years.
Acute ischemic cerebrovascular diseaseA total of 36 centers (87.8%) treated patients with ACVD of ischemic origin. The median (IQR) patients/year was 34 (70). The intensivist supervised initial care in only 16.7% of the centers, while the neurologist was in charge in 72.2%.
With regard to the organizational characteristics and the availability of procedures, 94.4% of the centers had a stroke/tele-stroke code, 72.2% were able to provide 24-h intraarterial thrombolysis/mechanical thrombectomy, and 83.3% were able to perform decompressive craniotomy in acute malignant middle cerebral artery disease of ischemic origin. Great variability was observed regarding the time limit for decompressive surgery: <24 h (12.9%); <48 h (29%); <72 h (19.4%); and no time limit (38.7%). A total of 63.9% of the centers had a specific management protocol, and 2.8% had participated in multicenter studies during the previous 5 years.
Our results are consistent with those found in the literature regarding the diagnosis of exclusion of aneurysm and the sealing of these lesions. Most of the centers (96.6%) performed the diagnosis of exclusion of aneurysm within the first 48 h. In the recently updated quality indicators of the SEMICYUC, indicator 35 addresses this issue, considering it necessary to reach 90% within the first 24 h.3 Although no direct comparison can be made because of the variations in time window, the survey responses obtained suggest good compliance in our Units. With regard to aneurysm management, the percentages obtained are in line with the data of the cerebrovascular disease group of the Spanish society of Neurosurgery,4 which evidence a predominance of endovascular treatment and an incidence of up to 17% of untreated aneurysms.
The management of blood pressure in ACVD of hemorrhagic origin is more controversial. Three treatment groups are contemplated. In 63.9% of the centers treatment was adjusted to a systolic blood pressure (SBP) target of 140–180 mmHg, while 33.3% sought a target of <140 mmHg. The INTERACT study compared a SBP target of 140 mmHg versus 180 mmHg, and found a pressure target of 140 mmHg to be associated to a decrease in hematoma growth without major side effects,5 defining it as a standard of care. Posteriorly, the ATACH-II study compared standard treatment (blood pressure 140–179 mmHg) versus intensive care (blood pressure 110–139 mmHg). No differences were observed between the two groups in terms of the neurological outcome, though the patients subjected to intensive care had a greater incidence of renal failure (9% versus 4%; p = 0.002).6 Thus, in our opinion an initial target of 140–180 mmHg seems reasonable, with more aggressive intervention in young individuals without comorbidities (in such cases a target of slightly under 140 mmHg may even be considered) and more permissive management (in the range of 160–180 mmHg) in older individuals, long-evolving hypertensive patients and subjects with important comorbidities.
In relation to ACVD of ischemic origin, the intensivist did not supervise initial management, which fundamentally corresponded to the neurologist. In addition, there was practically no participation of intensivists in multicenter studies. This evidences that with the exception of certain Departments of Intensive Care Medicine,7 the role of the intensivist in the initial management of ACVD of ischemic origin is very limited. We observed great variability in terms of the time limit for decompressive surgery. A recent study has shown that the earlier the intervention, the better the final outcome. Although a 48-h time window was suggested, the patient course was more closely related to the performance of hemi-craniectomy before herniation than to any concrete time window.8
Thanks are due to all the centers that completed the survey.
Please cite this article as: Llompart-Pou JA, Barea-Mendoza JA, Pérez-Bárcena J, Sánchez-Casado M, Ballesteros-Sanz MÁ, Chico-Fernández M. Encuesta de atención al paciente neurocrítico en España. Parte 2: Patología cerebrovascular. Med Intensiva. 2021;45:e1–e3.