The epidemiology of acute poisoning is highly variable and depends on multiple cultural, social, and geographical factors. Also, the type of toxics involved varies across time since the patterns of substance abuse also change, and new drugs appear.
In our setting we do not have data available on poisoned patients requiring admission to the ICU in the 21st century because the last nationwide study was published back in the 1980s.1
The objective of this paper is to know the epidemiology of poisoned patients requiring admission to the ICU during 2 different periods of time, and the variations that have occurred in both periods.
It is a 2-phase multicenter study. The first phase prospectively included poisoned patients who required ICU admission in 9 hospitals between 2002 and 2006. The second phase prospectively included poisoned patients admitted to 16 Spanish ICUs between 2013 and 2014.
Data analysis was performed using SAS® University Edition software. Data were analyzed using the chi-square test, the Cochran–Mantel–Haenszel test, the Breslow-Day test, and the Wilcoxon and Kolmogorov–Smirnov test. The categorical variables were expressed as n (%) and quantitative variables as mean (standard deviation).
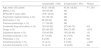
The first study phase included 340 patients and the second, 561. The rate of poisoned patients was 1.90% (561/29 600) of the patients admitted to these units during the second study period (data on the first period are not available). The demographic characteristics and types of toxic agents are shown on Table 1.
Characteristics and types of toxic agents.
| 1st period(N = 340) | 2nd period(N = 561) | Pvalue | |
|---|---|---|---|
| Age; mean (SD) years | 40.21 (16.06) | 45.34 (16.83) | P < .001 |
| Males; n (%) | 183 (53.98) | ND | |
| APACHE II; mean (SD) | 16.51 (8.02) | ND | |
| Psychiatric medical history; n (%) | 191 (56.18) | ND | |
| Alcoholism; n (%) | 86 (25.29) | ND | |
| Previous poisonings; n (%) | 111 (32.65) | ND | |
| Combined drug intoxication; n (%) | 183 (53.82) | 279 (49.73) | NS |
| Drugs; n (%) | 205 (60.29) | 396 (70.59) | .0015 |
| Substance abuse; n (%) | 139 (40.88) | 193 (34.40) | .05 |
| Domestic products; n (%) | 37 (10.88) | 44 (7.84) | NS |
| Pesticides; n (%) | 8 (2.35) | 8 (1.43) | NS |
| Industrial products; n (%) | 15 (4.41) | 2 (0.36) | <.0001 |
| Animals and plants; n (%) | 14 (4.12) | 16 (2.85) | NS |
NA, not available; NS, not significant; SD, standard deviation.
During the first period a total of 672 toxic agents/patient were reported, with a ratio of 1.98 toxic agents/patient. A total of 994 toxic agents (1.77 toxic agents/patient) were reported during the second period.
The most common toxic agents of each phase are shown on Table 2. The most common one in both periods were benzodiazepines, but the distribution of other toxic agents has changed significantly. Alcohol intoxication has improved (P = .0002), and in up to 60 cases (48%) it is the only toxic agent involved, which represents 10.70% of the patients from the second period.
Most common toxic agents by periods.
| 1st period(N = 735) | 2nd period(N = 994) | |
|---|---|---|
| 1 | Benzodiazepines, 121 (16.46%) | Benzodiazepines, 209 (21.03%) |
| 2 | Cocaine, 67 (9.12%)* | Ethanol, 125 (12.58%)* |
| 3 | Analogs to opioid receptors, 65 (8.84%)* | Neuroleptic agents, 80 (8.05%) |
| 4 | Neuroleptic agents, 55 (7.76%) | Tricyclic antidepressants, 67 (6.74%) |
| 5 | Heroine, 44 (5.10%)* | SSRT, 66 (6.64%)* |
| 6 | Ethanol, 42 (5.71%)* | Analogs to opioid receptors, 57 (5.73%)* |
| 7 | Tricyclic antidepressants, 42 (5.85%) | Cannabis, 38 (3.82%) |
| 8 | Methadone, 24 (2.66%) | Cocaine, 36 (3.62%)* |
| 9 | SSRT, 21 (2.66%) | Paracetamol, 35 (3.52%) |
| 10 | Lithium, 18 (2.45%)* | Oral antidiabetics, 24 (2.41%)* |
SSRI, selective serotonin reuptake inhibitors.
Data expressed as no. (percentage with respect to the total number of toxic agents).
In both periods, around half of the patients had used more than just 1 toxic agent. The most common ones associated with other toxic agents were psychoactive medications and substance abuse. Although the distribution varies between both periods, the only significant difference was found in the increased rate of acute alcohol intoxications with ethanol (21.43 vs. 48%; P = .007).
The intentionality of poisoning within the first period was self-harm in 172 patients (46.11%), accidental in 62 (16.62%), and recreational in 96 (28.24%). The intentionality within the second period was never recorded.
Regarding specific treatments, during the first period, 132 patients received selective digestive decontamination (38.82%), 202 received antidotes (59.41%), and 24 patients received extrarenal blood purification techniques (7.06%). Regarding the second period, 184 patients received selective digestive decontamination (32.80%), 283 patients received antidotes (52.02%), and 42 received extrarenal blood purification techniques (8.32%) without significant differences between both study periods.
The mortality rate at the ICU setting was 10.53% (32 patients) during the first study period, and 6.06% (34 patients) during the second period (P = .018).
Acute poisonings are still a rare entity at the ICU setting. Although the distribution of the different toxic agents has not changed significantly, an increase of drug poisoning, especially psychoactive drugs, has been reported. Also, there has been a change in substance abuse habits as confirmed by the increase of alcohol intoxications that has almost doubled, especially acute alcohol intoxications, suggestive of changes in the admission criteria or, more likely, indicative of the consumption of greater amounts of alcohol. However, opioid poisoning has dropped, although it has gone up in countries like the United States.2,3
The evolution of both alcohol and heroin use is associated with the data shown in the 2018 report published by the Spanish Observatory on Drugs and Addictions.4 Although we there are no data available on the study period since the EDADES survey was collected for the last time, it seems that in our setting opioid abuse is not a problem,5 which would explain the differences seen with respect to the United States.
The increased substance abuse is also evident on the medical literature available,6,7 especially due to the involuntary poisonings of polymedicated elderly patients. Although the second period of the study did not include the intentionality of poisoning, the population older age may have something to do with this.
On the other hand, mortality rate is high in both study periods compared to data from other neighboring countries with mortality rates around 2%.8,9 Still, the mortality rate has dropped 42% between the 2 periods studied down to rates similar to the ones described by the last multicenter study on Spanish ICUs published in 1983.1 The higher prevalence of poisoning due to industrial products seen within the first period can be the reason behind such a high mortality rate. Still, in the future, the adequacy of the therapies administered should be studied in close detail.
Our study main limitation is that, although some centers participate in both periods, others only did so in one study period. This means that geographic variability may explain some of the differences seen. Also, no incidence rate of this type of disease with respect to ICU admissions was collected within the first study period. No past medical history, severity or sex distribution was collected within the second study period either.
Although most of the poisonings that end up in the Spanish ICUs are due to psychoactive drugs, there are differences in the types of toxic agents involved in relation to the different patterns of consumption. Some of them probably reflect the appearance of dangerous patterns of consumption as in the case of ethanol and other possible medication errors or interactions in polymedicated patients although this still needs to be confirmed in further studies. However, our specialty is unconnected to the epidemic of deaths due to opioids seen in the United States.
This study is part of a PhD program in psychiatry conducted at Universitat Autònoma de Barcelona, Spain.
Hospital Vall d’Hebrón: Francisco Javier Montero Clavero, Antonia Socias Mir, Rosa Alcaraz Peñarrocha, and Jaime Baldirà Martínez de Irujo; Hospital Clínic de Barcelona: Santiago Nogué Xarau; Hospital Sant Pau: Luís Marruecos Sant, and Indalecio Morán Chorro; Hospital del Mar: Joan Nolla Salas; Hospital Josep Trueta: Sandra Barbadillo Ansorregui; Hospital Joan XXIII: Elisabet García Mañosa; Mutua de Terrassa: J. Martínez; Hospital Clínico de Zaragoza: Emilia Civeira Murillo; Hospital Universitario Son Llàtzer: Antonia Socias Mir, Inmaculada de Dios Chacón, and Sara Franco Serrano; Hospital Verge de la Cinta: Ferrán Roche-Campo; Hospital Marqués de Valdecilla: Ana García Miguélez; Complejo Hospitalario Universitario de Orense: Jesús Priego Sanz; Hospital Universitario del Henares: Teresa Mozo Martín; Hospital Príncipe de Asturias: Madian Manso Álvarez; Hospital Universitario de Albacete: Mirian Gimeno González; Complejo Hospitalario Universitario de Ferrol: Carmen J Fernández González; Hospital Álvaro Cunqueiro: Isabel Gallego Barbáchano, and María José Rodríguez Fernández; Hospital Universitario Río Hortega: Marta García García, and Pablo Blanco Sweizer; Hospital Universitari Sant Joan de Reus: Elisabet García Mañosa; Hospital Universitario Arnau de Vilanova (Lleida): Mercedes Palomar Martínez, and Sulamita Carvalho Brugger; and Hospital Universitario Arnau de Vilanova Universitario Araba: Sergio Castaño Ávila.
Please cite this article as: Socias Mir A, Nogué Xarau S, Alcaraz Peñarrocha RM, Morán Chorro I, Montero Clavero FJ, Palomar Martínez M, et al. Evolución de las intoxicaciones en las unidades de cuidados intensivos españolas: comparación de 2 periodos. Med Intensiva. 2021;45:e4–e6.
The names of the members from SEMICYUC Toxicology Working Group and the participants of EMPIUCI 13-14 are shown in Appendix A.